Anatomy and Physiology of Reproductive System
Subject: Gynecological Nursing

Overview
Male Reproductive System
The reproductive organs are what make up the male reproductive system, just like the female reproductive system. The male reproductive system is specifically adapted to produce and maintain male sex cells, or sperm, transfer those cells along with supportive fluids to the female reproductive system, and release the male hormone testosterone. The male reproductive system is made up of the penis, scrotum, two testes (where sperm cells and testosterone are produced), and accessory organs.
The functions of the male reproductive system are:
- Spermatozoa transfer to the female
- production of spermatozoa and male gametes
Penis
The penis is the site of copulation and serves as both a sperm exit and a urine exit. The skin of the penis is thin and hairless. The prepuce, commonly known as the foreskin, is a circular fold of skin that covers the glands unless it is removed through circumcision soon after birth. The urinary meatus, which is located near the tip of the penis, serves as the urethra's external opening. Erectile tissue makes up the majority of the penis' tissue. Most of the body of the penis is composed of three cylindrical spaces (sinuses) filled with erectile tissue.
The two bigger ones, referred known as corpora cavernosa, are close by. The urethra is encircled by the corpus spongiosum, the third sinus. Erection happens when nerve impulses from the autonomic nervous system dilate the arteries.
The corpus spongiosum, the third sinus, surrounds the urethra. Nerve impulses from the autonomic nervous system can widen the arteries of the penis, allowing arterial blood to flow into the organ's erectile tissues and resulting in an erection. The skin of the penis is flexible and elastic to accommodate changes in penile size during an erection.
Semen, which contains sperm (reproductive cells), is released (ejaculated) through the end of the penis when a man experiences sexual climax. The urethra cannot drain urine during an orgasm while the penis is erect, so only semen can be ejaculated.
Scrotum
The pouch with thin skin that encloses and guards the testes is called the scrotum. Because optimal sperm production requires the testes to be just a little bit colder than body temperature, the scrotum also serves as a climate control system for them. The testes can hang farther from the body to cool or be pulled closer to the body for warmth or protection by relaxing or contracting the cremaster muscles in the scrotal wall. The scrotum is divided into two chambers, each of which contains a testis, by a medial septum.
The spermatic cord, which connects the testicles at either end, secures the oval organs in the scrotum, which are about the size of huge olives. Men often have two testicles. The testes are where sperm and testosterone, the main hormone involved in male sex, are produced. Seminiferous tubules, coiling collections of tubes, are found inside the testes. Sperm cells are generated by means of these tubes.
Internal Male Reproductive Organ
The internal structures include the testes, the ductal system, and accessory glands.
Testes
The testes are oval, scrotum-located bodies about the size of large olives; typically, the left testis hangs a little lower than the right.
The production of sperm and the synthesis of testosterone are the two jobs of the testes (the primary male sex hormone). The testes' seminiferous tubules are where sperm is made. The anterior pituitary releases the gonadotropins FSH and LH, which function similarly to the female reproductive system. These hormones promote the production of testosterone in the testes, which helps to maintain spermatogenesis and boosts sperm production in the seminiferous tubules as well as seminal fluid production. The epididymis is a coiled tube that is over 20 feet long and rests up against the testicles. It gathers sperm from the testes and gives sperm the room and environment they need to develop.
The Ductal System
The vas deferens is a cord-like duct that transports sperm from the epididymis. One such duct travels from each testis up to the back of the prostate and enters the urethra to form the ejaculatory ducts. Other structures, such as blood vessels and nerves, also travel along with each vas deferens and together form the spermatic cord. The urethra is the terminal duct of the reproductive and urinary systems, serving as a passageway for semen (fluid containing sperm) and urine. It passes through the prostate gland and the penis and opens to the outside.
Accessory Glands
The seminal vesicles, which produce nutrient seminal fluid, and the prostate gland, which produces alkaline prostatic fluid, are both connected to the ejaculatory duct leading into the urethra. The paired seminal vesicles are convoluted pouch-like structures lying posterior to, and at the base of, the urinary bladder in front of the rectum. They secrete an alkaline fluid that contains fructose and prostaglandins. The fructose supplies energy to the sperm on its journey to meet the ovum, and the prostaglandins assist in sperm mobility.
The prostate gland lies just under the bladder in the pelvis and surrounds the middle portion of the urethra. Usually the size of a walnut, this gland enlarges with age. The prostate and the seminal vesicles above it produce fluid that nourishes the sperm. This fluid provides most of the volume of semen, the secretion in which sperm are expelled during ejaculation. Other fluid that makes up the semen comes from the vas deferens and from mucous glands in the head of the penis.
The bulbourethral glands (Cowper's glands) are two small structures about the size of peas, located inferior to the prostate gland. They are composed of several tubes whose epithelial linings secret a mucus-like fluid. It is released in response to sexual stimulation and lubricates the head of the penis in preparation for sexual intercourse. Their existence is said to be constant, but they gradually diminish in size with advancing age.
Male Sexual Response
Regardless of the type of sexual stimulation, the physiologic response in both men and women is similar and usually follows a four-phase pattern:
- Excitement: The person experiences sexual arousal with specific changes such as the erection of the penis in males.
- Plateau: Physiologic changes of the excitement phase level off.
- Orgasm: The tension that built up during the previous two phases is released.
- Resolution: The body returns to the physiologic nonstimulated state.
Sexual behavior involves the participation of autonomic and somatic nerves and the integration of numerous spinal sites in the central nervous system (CNS). The penile portion of the process that leads to erections represents only a single component. Penile erections are an integration of complex physiologic processes involving the CNS, peripheral nervous system, and hormonal and vascular systems. With sexual stimulation, the arteries leading to the penis dilate and increase blood flow into erectile tissues. At the same time, the erectile tissue compresses the veins of the penis, reducing blood flow away from the penis. Blood accumulates, causing the penis to swell and elongate and producing an erection
As in women, the culmination of sexual stimulation is an orgasm, a pleasurable feeling of physiologic and psychological release. Orgasm is accompanied by emission (movement of sperm from the testes and fluids from the accessory glands) into the urethra, where the sperm and fluids are mixed to form semen. As the urethra fills with semen, the base of the erect penis contracts, which increases pressure. This pressure forces the semen through the urethra to the outside (ejaculation). During ejaculation, the ducts of the testes, epididymis, and vas deferens contract and cause expulsion of sperm into the urethra, where the sperm mixes with the seminal and prostatic fluids. These substances, together with mucus secreted by accessory gland.
FEMALE REPRODUCTIVE SYSTEM
The functions of the female reproductive system are:
- Formation of female gametes, ova
- Reception of male gametes, spermatozoa
- Provision of suitable environments for fertilization of the ovum by spermatozoa and development of the resultant fetus Parturition (childbirth)
- Lactation, the production of breast milk, which provides complete nourishment for the baby in its early life.
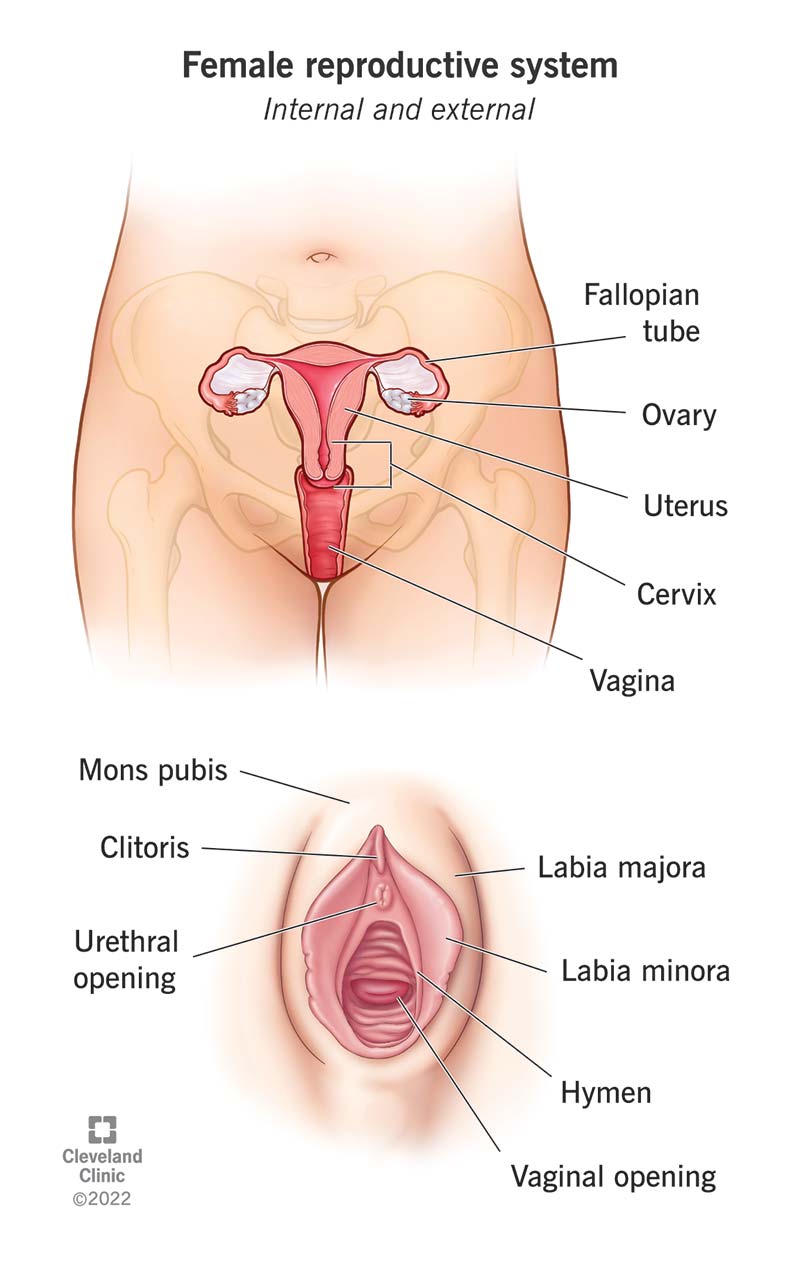
External Genitalia (Vulva)
The external genitalia are known collectively as the vulva, and consist of the labia majora and labia minora, the clitoris, the vaginal orifice, the vestibule, the hymen and the vestibular glands (Bartholin's glands).
Labia majora: These are the two large folds which form the boundary of the vulva. They are composed of skin, fibrous tissue and fat and contain large numbers of sebaceous glands. Anteriorly the folds join in front of the symphysis pubis, and posteriorly they merge with the skin of the perineum. At puberty hair grows on the mons pubis and on the lateral surfaces of the labia majora.
Labia minora: These are two smaller folds of skin between the labia majora, containing numerous sebaceous glands. The cleft between the labia minora is the vestibule. The vagina, urethra and ducts of the greater vestibular glands open into the vestibule.
Clitoris: The clitoris corresponds to the penis in the male and contains sensory nerve endings and erectile tissue but it has no reproductive significance.
Vestibular glands: The vestibular glands (Bartholin's glands) are situated one on each side near the vaginal opening. They are about the size of a small pea and have ducts, opening into the vestibule immediately lateral to the attachment of the hymen. They secrete mucus that keeps the vulva moist.
Fourchette: Fourchette created as the labia majora join posteriorly to the vaginal orifice. is a distinct landmark that should be identified for correct perineal alignment during perinea! suturing.
Perineum Extends from the fourchette to the anal margin, covering the pelvic floor muscles It is composed of the levator ani muscle and fascia, the deep perineal muscles and the external genitalia muscles. These muscles function as supports to the pelvic organs. The pudendal arteries veins and nervous supply the muscles, foscia and skin of the perineim.
Prepuce: It is a loose fold of skin covering the clitoris.
Frenulum: A small ligament maintaining the position of the clitoris.
The vulval blood supply: This comes from the internal and external pudendal arteries. The blood drains through corresponding veins,
Nerve Supply: This is derived from branches of the pudendal nerve. The vaginal nerves supply the erectile tissue of the estibular bulbs and clitoris and their parasympathetic fibres have a vasodilator effect.
Lymphatic drainage: This is mainly via the inguinal gland.
Blood Supply, Lymph Drainage and Nerve Supply
The arterial supply: This is by branches from the internal pudendal arteries that branch from the internal iliac arteries and by external pudendal arteries that branch from the femoral arteries.
The venous drainage: This forms a large plexus which eventually drains into the internal iliac veins.
Lymph drainage: This is through the superficial inguinal nodes.
Nerve supply: This is by branches from pudendal nerves.
Perineum: The perineum is the area extending from the base of the labia minora to the anal canal. It is roughly triangular and consists of connective tissue, muscle and fat. It gives attachment to the muscles of the pelvic floor.
Internal Female Reproductive Organ
The internal female reproductive organs consist of the vagina, uterus, fallopian tubes, and ovaries. These structures develop and function according to specific hormonal influences that affect fertility and childbearing
Vagina
The vagina is a highly distensible canal situated in front of the rectum and behind the bladder. It is a tubular, fibromuscular organ lined with mucous membrane that lies in a series of transverse folds called rugae. The rugae allow for extreme dilation of the canal during labor and birth. The vagina is a canal that connects the external genitals to the uterus. It receives the penis and the sperm ejaculated during sexual intercourse, and it serves as an exit passageway for menstrual blood and for the fetus during childbirth. The front and back walls normally touch each other so that there is no space in the vagina except when it is opened (e.g., during a pelvic examination or intercourse). In the adult, the vaginal cavity is 3 to 4 inches long. Muscles that control its diameter surround the lower third of the vagina. The upper two third of the vagina lies above these muscles and can be stretched easily.
During a woman's reproductive years, the mucosal lining of the vagina has a corrugated appearance and is resistant to bacterial colonization. Before puberty and after menopause (if the woman is not taking estrogen), the mucosa is smooth due to lower levels of estrogen. The vagina has an acidic environment, which protects it against ascending infections. Antibiotic therapy, douching, perineal hygiene sprays, and deodorants upset the acid balance within the vaginal environment and can predispose women to infections.
Uterus
The uterus is a pear-shaped muscular organ at the top of the vagina. It lies behind the bladder and in front of the rectum and is anchored in position by eight ligaments, although it is not firmly attached or adherent to any part of the skeleton. A full bladder tilts the uterus backward; a distended rectum tilts it forward. The uterus alters its position by gravity or with change of posture, and is the size and shape of an inverted pear. It is the site of menstruation, implantation of a fertilized ovum, development of the fetus during pregnancy, and labor. Before the first pregnancy, it measures approximately 3 inches long, 2 inches wide, and 1 inch thick. After a pregnancy, the uterus remains larger than before the pregnancy. After menopause, it becomes smaller and atrophies.
The parts of the uterus are the fundus, body and cervix
The fundus: This is the dome-shaped part of the uterus above the openings of the uterine tubes.
The body: This is the main part. It is narrowest inferiorly at the internal os where it is continuous with the cervix.
The cervix ('neck' of the uterus). This protrudes through the anterior wall of the vagina, opening into it at the external os.
Uterus
Structure of the Uterus
The walls of the uterus are composed of three layers of tissue: perimetrium, myometrium and endometrium.
Perimetrium
This is peritoneum, which is distributed differently on the various surfaces of the uterus Anteriorly it extends over the fundus and the body where it is folded on to the upper surface of the extends over the fundus, the body and the cervix, then it continues on to the rectum to form the rectouterine pouch (of Douglas), Laterally only the fundus is covered because the peritoneum forms a double fold with the uterine tubes in the upper free border. This double fold is the broad ligament which, at its lateral ends, attaches the uterus to the sides of the pelvis.
Myometrium:
This is the thickest layer of tissue in the uterine wall. It is a mass of smooth muscle fibres interlaced with areolar tissue, blood vessels and nerves.
Endometrium:
This consists of columnar epithelium containing a large number of mucus-secreting tubular glands. It is divided functionally into two layers.
- The functional layer is the upper layer and it thickens and becomes rich in blood vessels in the first half of the menstrual cycle. If the ovum is not fertilised and does not implant, this layer is shed during menstruation.
- The basal layer lies next to the myometrium, and is not lost during menstruation. It is the layer from which the fresh functional layer is regenerated during each cycle.
The upper two-thirds of the cervical canal is lined with this mucous membrane.
Further towards the vagina, however, the mucosa changes, becoming stratified squamous epithelium, which is continuous with the lining of the vagina itself.
Blood Supply, Lymph Drainage and Nerve Supply
The Arterial supply: This is by the uterine arteries which are branches of the internal iliac arteries.
They pass up the lateral aspects of the uterus between the two layers of the broad ligaments.
They supply the uterus and uterine tubes and join with the ovarian arteries to supply the ovaries. Branches pass downwards to anastomose with the vaginal arteries to supply the vagina.
Venous drainage: The veins follow the same route as the arteries and eventually drain into
the internal iliac veins.
Lymph drainage: There are deep and superficial lymph vessels which drain lymph from the uterus and the uterine tubes to the aortic lymph nodes and groups of nodes associated with the iliac blood vessels.
Nervesupply: The nerves supplying the uterus and the uterine tubes consist of parasympathetic fibres from the sacral outflow and sympathetic fibres from the lumbar outflow.
Supports of the Uterus
The uterus is supported in the pelvic cavity by surrounding organs, muscles of the pelvic floor and ligaments that suspend it from the walls of the pelvis.
Supporting Structures
The broad ligaments: These are formed by a double fold of peritoneum, one on each side of the uterus. They hang down from the uterine tubes as though draped over them and at their lateral ends they are attached to the sides of the pelvis. The uterine tubes are enclosed in the upper free border and near the lateral ends they penetrate the posterior wall of the broad ligament and open into the peritoneal cavity. The ovaries are attached to the posterior wall, one on each side. Blood and lymph vessels and nerves pass to the uterus and uterine tubes between the layers of the broad ligaments.
The round ligaments: These are bands of fibrous tissue between the two layers of broad ligament, canal to end by fusing with the labia majora.
The uterosacral ligaments: These originate from the posterior walls of the cervix and vagina and extend backwards, one on each side of the rectum, to the sacrum.
The transverse cervical ligaments (cardinal ligaments): These extend one from each side of the cervix and vagina to the side walls of the pelvis.
The pubocervical fascia: This extends forward from the transverse cervical ligaments on each side of the bladder and is attached to the posterior surface of the pubic bones.
Functions of the Uterus
The uterus has several important functions in the body including multiple reproductive functions such as implantation, gestation, labor, delivery and menses. When an egg is releases from an ovary, it travels along the fallopian tube which is where a sperm cell will fertilize it (if it becomes fertilized). The endometrial layer of the uterus thickens to provide the fertilized egg a location to implant in. If the egg is not fertilized, however, menstrual bleeding occurs due to the endometrial layer dissolving and going out through the vagina. Because of this, the uterus or womb is responsible for the menstrual cycle and the beginning of these menses is one of the signs of puberty.
The uterus also responds to hormones, directing the blood that flows towards the vagina. During intercourse, the uterus contracts and this helps the sperm reach the fallopian tubes. The uterus plays a role in both regular menses and reproduction.
As mentioned, an egg that is fertilized in one of the fallopian tubes will enter the uterus and be implanted in the endometrial lining. Then the womb provides nourishment allowing the egg to grow into a fetus and continue to develop during gestation. The uterus is incredibly elastic and as the fetus develops, the womb will stretch to hold not only the baby, but also the placenta and a liter of amniotic fluids. The uterus also gives structural support for both the bladder and the bowels.
The uterus is also designed so that its contracts make childbirth easier. During pregnancy, the cervix (which is part of the uterus) is closed and remains thick. When labor approaches, however, the womb begins to contract and the cervix is pulled upwards. Eventually the contractions lead to the cervix dilating fully reaching a diameter of 10 centimeters to accommodate the baby's head. Additional pressure from the uterus is applied during labor and this is what pushes the baby downward, leading to birth.
Cervix
The cervix, the lower part of the uterus, opens into the vagina and has a channel that allows sperm to enter the uterus and menstrual discharge to exit. It is composed of fibrous connective tissue.
During a pelvic examination, the part of the cervix that protrudes into the upper end of the vagina can be visualized. Like the vagina, this part of the cervix is covered by mucosa, which is smooth, firm, and doughnut shaped, with a visible central opening called the external os. Before childbirth, the external cervical os is a small, regular, oval opening. After childbirth, the opening is converted into a transverse slit that resembles lips. Except during menstruation or ovulation, the cervix is usually a good barrier against bacteria. The cervix has an alkaline environment, which protects the sperm from the acidic environment in the vagina.
The canal or channel of the cervix is lined with mucus-secreting glands. This mucus is thick and impenetrable to sperm until just before the ovaries release an egg (ovulation). At ovulation, the consistency of the mucus changes so that sperm can swim through it, allowing fertilization. At the same time, the mucus secreting glands of the cervix actually become able to store live sperm for 2 or 3 days. These sperm can later move up through the corpus and into the fallopian tubes to fertilize the egg; thus, intercourse 1 or 2 days before ovulation can lead to pregnancy. Because some women do not ovulate consistently, pregnancy can occur at varying times after the last menstrual period. The channel in the cervix is too narrow for the fetus to pass through during pregnancy, but during labor it stretches to let the newborn through.
Corpus:
The corpus, or the main body of the uterus, is a highly muscular organ that enlarges to hold the fetus during pregnancy. The inner lining of the corpus (endometrium) undergoes cyclic changes as a result of the changing levels of hormones secreted by the ovaries: it is thickest during the part of the menstrual cycle in which a fertilized egg would be expected to enter the uterus and is thinnest just after menstruation. If fertilization does not take place during this cycle, most of the endometrium is shed and bleeding occurs, resulting in the monthly period. If fertilization does take place, the embryo attaches to the wall of the uterus, where it becomes embedded in the endometrium (about 1 week after fertilization); this process is called implantation. Menstruation then ceases during the 40 weeks (280 days) of pregnancy. During labor, the muscular walls of the corpus contract to push the baby through the cervix and into the vagina.
Fallopian Tubes/Uterine tube
Each fallopian tube is attached to the uterine cornu and passes outwards and backwards in the upper part of the broad ligament. The fallopian tube measures 4 inch (10 cm) or more in length. The fallopian tube is divided anatomically into four parts:
1. The interstitial portion is the innermost part of the tube which traverses the myometrium to and approximately 8 mm in diameter, but the diameter diminishes near the cornu of the uterus to 1 mm into the endometrial cavity. It is the shortest part of the tube, its length being the thickness of the uterine muscle, about 18 mm. It is also the narrowest part, its internal diameter being 1 mm or less so that only the finest cannula can be passed into it during falloscopy examination. There are no longitudinal muscle fibres here but the circular fibres are well developed.
2. The isthmus comprises the next and inner part of the tube and represents about one-third of the total length, i.e. 35 mm. It is narrow but a little wider than the interstitial part and its lumen has a diameter of 2 mm. Its muscle wall contains both longitudinal and circular fibres, and it is covered by peritoneum except for a small inferior bare area related to the broad ligament. It is relatively straight..
3. The ampulla is the lateral, widest and longest part of the tube and comprises roughly two-thirds of the tube, measuring 2.5-3 inch (60-75 mm) in length. Here the mucosa is arborescent with many complex folds. Fertilization occurs in the ampullary portion of the fallopian tube.
4. The fimbriated extremity or infundibulum is where the abdominal ostium opens into the peritoneal cavity. The fimbriae are motile and almost prehensile, and enjoy a considerable range of movement and action. One fimbria - the ovarian fimbria - is larger and longer than the others and is attached to the region of the ovary. This fimbria embraces the ovary at ovulation, picks up the ovum and carries it to the ampullary portion.
Layers of fallopian tube
1. Serous layer
2. Muscular layer and
3. Mucus membrane
The Ovaries
Each ovary weighs 4-8 g and measures about 35 mm in length, 25 mm in width and 18 mm in thickness The ovary is almond shaped, pearly grey due to a compact tunica albuginea, and the surface is slightly corrugated. Before puberty, the ovaries are small and located near the pelvic brim. After menopause they atrophy and become shrunken and the grooves and furrows on the surface become well marked An ovary larger than this as measured ultrasonically.
Structure of the Ovaries
- The ovaries have two layers of tissue.
The medulla
- This lies in the centre and consists of fibrous tissue, blood vessels and nerves.
The cortex
This surrounds the medulla. It has a framework of connective tissue, or stroma, covered by germinal epithelium. It contains ovarian follicles in various stages of maturity, each of which contains an ovum Before puberty the ovaries are inactive but the stroma already contains immature (primordial) follicles, which the female has from birth. During the childbearing years, about every 28 days, one ovarian follicle (Graafian follicle) matures, ruptures and releases its ovum into the peritoneal cavity. This is called ovulation and it occurs during most menstrual cycles.
Blood Supply, Lymph Drainage and Nerve Supply
Arterial supply: This is by the ovarian arteries, which branch from the abdominal aorta just below the renal arteries.
Venous drainage: This is into a plexus of veins behind the uterus from which the ovarian veins arise. The right ovarian vein opens into the inferior vena cava and the left into the left renal vein.
Lymph drainage: This is to the lateral aortic and preaortic lymph nodes. The lymph vessels follow the same route as the arteries.
Nerve supply: The ovaries are supplied by parasympathetic nerves from the sacral sympathetic nerves from the lumbar outflow.
BREASTS
The two mammary glands, or breasts, are accessory organs of the female reproductive system that are specialized to secrete milk following pregnancy.
They overlie the pectoralis major muscles and extend from the second to the sixth ribs and from the sternum to the axilla. Each breast has a nipple located near the tip, which is surrounded by a circular area of pigmented skin called the areola.
Each breast is composed of approximately 9 lobes (the number can range between 4 and 18), which contain glands (alveolar) and a duct (lactiferous) that leads to the nipple and opens to the outside. The lobes are separated by dense connective and adipose tissues, which also help support the weight of the breasts.
Structure of the Breast
The mammary glands consist of glandular tissue, fibrous tissue and fatty tissue. Each breast consists of about 20 lobes of glandular tissue, each lobe being made up of a number of lobules that radiate around the nipple. The lobules consist of a cluster of alveoli which open into small ducts and these unite to form large excretory ducts, called lactiferous ducts. The lactiferous ducts converge towards the centre of the breast where they form dilatations or reservoirs for milk. Leading from each dilatation, or lactiferous sinus, is a narrow duct which opens on to the surface at the nipple. Fibrous tissue supports the glandular tissue and ducts, and fat covers the surface of the gland and is found between the lobes.
The Nipple
This is a small conical eminence at the centre of the breast surrounded by a pigmented area, the areola.
On the surface of the areola are numerous sebaceous glands (Montgomery's tubercles) which lubricate the nipple during lactation
Blood Supply, Lymph Drainage and Nerve Supply
Arterial blood supply. The breasts are supplied with blood from the thoracic branches of the axillary arteries and from the internal mammary and intercostal arteries
. Venous drainage: This describes an anastomotic circle round the base of the nipple from which branches carry the venous blood to the circumference and end in the axillary and mammary veins.
Lymph drainage: This is mainly into the axillary lymph vessels and nodes, Lymph may drain through the internal mammary nodes if the superficial route is obstructed.
Nerve supply: The breasts are supplied by branches from the 4th, 5th and 6th thoracic nerves which contain sympathetic fibres. There are numerous somatic sensory nerve endings in the breast especially around the nipple. When these touch receptors are stimulated by sucking, impulses pass to the hypothalamus and the flow of the hormone oxytocin is increased, promoting the release of milk.
Function of the Breast
During pregnancy, placental estrogen and progesterone stimulate the development of the mammary glands. Because of this hormonal activity, the breasts may double in size during pregnancy. At the same time, glandular tissue replaces the adipose tissue of the breasts. Following childbirth and the expulsion of the placenta, levels of placental hormones (progesterone and lactogen) fall rapidly, and the action of prolactin (milk producing hormone) is no longer inhibited. Prolactin stimulates the production of milk within a few days after childbirth, but in the interim, dark yellow fluid called colostrum is secreted. Colostrum contains more minerals and protein, but less sugar and fat, than mature breast milk. Colostrum secretion may continue for approximately a week after childbirth, with gradual conversion to mature milk. Colostrum is rich in maternal antibodies, especially immunoglobulin A (IgA), which offers protection for the newborn against enteric pathogens.
FEMALE PELVIS
The Female Bony Pelvis
The pelvis is a hard ring of bone, which supports and protects the pelvic organs and the contents of the abdominal cavity. The muscles of the legs, back and abdomen are attached to the pelvis, and their strength and power keep the body upright and enable it to bend and twist at the waist, and to walk and run. The woman's pelvis is adapted for child bearing, and is a wider and flatter shape than the male pelvis
The pelvis is composed of pairs of bones, which are fused together so tightly that the joints are difficult to see during pregnancy, physiological process effects and bring changes in composition, shape, plane of inclination and internal dimensions of the true pelvis.
Function of Pelvis
- Supports the weight of the body through the vertebral column and passes that force onto the hipbones
- Receives ground forces during walking and transmits them upward toward the vertebral column
- Supports and protects pelvis viscera
- Provides attachment site for muscles
- Makes up bony portion of birth canal
The pelvis consists of pelvic bones;
- Two innominate bone
- One sacrum
- One coccyx
Ilium: The major portion of the pelvis is composed of two bones, each called the ilium - one on either side of the backbone (or spinal column) and curving towards the front of the body. When you place your hand on either hip, your hand rests on the iliac crest, which is the upper border of the ilium on that side. At the front of the iliac crest, you can feel the bony protuberance called the anterior superior iliac spine (a 'protuberance' is something that sticks out, like a little hill or knob).
Ischium: The ischium is the thick lower part of the pelvis, formed from two fused bones - one on either side. When a woman is in labour, the descent of the fetal head as it moves down the birth canal is estimated in relation to the ischial spines, which are inward projections of the ischium on each side. The ischial spines are smaller and rounder in shape in the woman's pelvis than in that of the man.
Pubic bones and the symphysis pubis: The pubic bones on either side form the front part of the pelvis. The two pubic bones meet in the middle at the pubic symphysis. (A symphysis is a very strong bony joint.) The pubic symphysis is immediately below the hair-covered pubic mound that protects the woman's external genitalia. When you examine the abdomen of a pregnant woman, feeling for the top of the pubic symphysis with your fingers is a very important landmark.
Sacrum: The sacrum is a tapered, wedge-shaped bone at the back of the pelvis, consisting of five fused vertebrae (the small bones that make up the spinal column or backbone). The border of the first vertebra in the sacrum sticks out, and points towards the front of the body; this protuberance is the sacral promontory - an important landmark for labour and delivery.
Coccyx: The coccyx, also known as the tailbone, is a small, triangular bone resembling a shortened tail located at the bottom of the spine. It is composed of three to five coccygeal vertebrae or spinal bones. The vertebrae may be fused together to form a single bone; however, in some cases, the first vertebra is separate from the others.
The coccyx is connected to the sacrum by means of an amphiarthrodial joint. This is a type of joint that functionally only allows for a slight amount of movement. Later in life, the coccyx may fuse with the sacrum, though this is more common in women than in men. The coccyx serves as an attachment site for tendons, ligaments, and muscles. It also functions as an insertion point of some of the muscles of the pelvic floor. The coccyx also functions to support and stabilize a person while he or she is in a sitting position. A woman's coccyx may be broken during a complicated childbirth. A qualified medical professional may prescribe pain medication until the coccyx heals. In extreme cases, the coccyx may need to be surgically removed. This procedure is called a coccygectomy.
Pelvic Joints
There are four pelvic joints -one symphysis pubis, two sacroiliac joints and one sacro-coccygeal joint. In the non-pregnant state there is very little movement in these joints, but during pregnancy endocrine activity causes the ligaments to soften, which allows the joints to give. This may provide more room for the fetal head as it passes through the pelvis. The symphysis pubis may separate slightly in later pregnancy. If it widens appreciably, the degree of movement permitted may give rise to pain on walking. The sacro-coccygeal joint permits coccyx to the deflected backward during the birth of the head.
The four pelvic joints are:
- One symphysis pubis
- Two sacroiliac joints
- One sacro-coccygeal joint
The symphysis pubis is formed at the junction of the two pubic bones, which are united by a pad of cartilage.
The sacroiliac joints: These are the strongest joints in the body. They join the sacrum to the ilium and thus connect the spine to the pelvis.
The sacro coccygeal joint: This joint is formed where the base of the coccyx articulate with the tip of the sacrum.
In the non-pregnant state there is very little movement in these joints, but during pregnancy endocrine activity causes the ligaments to soften, which allows the joints to move. This may provide more room for the fetal head as it passes through the pelvis. The symphysis pubis may separate slightly in later pregnancy. If it widens appreciably, the degree of movement permitted may give rise to pain on walking. The sacro-coccygeal joint permits coccyx to the deflected backward during the birth of the head.
Pelvic Ligaments
Each of the pelvic joints is held together by ligaments
- Interpubic ligaments at the symphysis pubis
- Sacro-iliac ligaments
- Sacro-coccygeal ligaments
There are other other ligaments ligaments important in midwifery
- The sacro-tuberous ligament
- The sacro-spinous ligament
The sacro-tuberous ligament runs from the sacrum to the ischial tuberosity and the sacro-spinous Acetabulum ligament from the sacrum to the ischial spine. These two ligaments cross the sciatic notch and from the posterior wall of the pelvic outlet.
The False Pelvis and the True Pelvis
The pelvis is divided by the linea terminalis into the false pelvis above this demarcation and the true pelvis below it. The true pelvis constitutes the bony passageway through which the fetus must maneuver to be born vaginally. Therefore, its construction, planes, and diameters are of utmost obstetric importance. The true pelvis has five boundaries:
Superiorly: The sacral promontory, linea terminalis, the upper margins of the pubic bones.
Posteriorly: The anterior surface of the sacrum and coccyx.
Inferiorly: The inferior margins of the ischial tuberosities and the tip of the coccyx.
Laterally: The sacroiliac notches and ligaments and the inner surface of the ischial bones.
Anteriorly: The obturator foramina, and the posterior surfaces of the symphysis pubis, pubic bones, and ascending rami of the ischial bones.
Female pelvis
False pelvis is shallow cavity above the inlet, true pelvis is deeper position of cavity below the inlet The true pelvis has three parts namely brim, a cavity and an outlet.
The Pelvic Inlet/ Brim
The brim or inlet The pelvic inlet (superior strait) is the upper entry into the true pelvis. Its boundaries are the sacral promontory posteriorly. the linea terminalis laterally, and the upper portion of the symphysis pubis and horizontal rami of the pubic bones anteriorly.
The shape of the pelvic inlet is transversely oval. with a slight posterior indentation caused by the sacral promontory.
Land marks of the brim: the inlet has the landmarks, these are the fixed anatomical points: on the brim.
1. Sacral promontory
2. Sacral wing or sacral ala
3. Sacro-iliac joint
4. The ileo-pectineal line- the edge formed at the inward aspect of the ilium
5. The ilio-pectineal eminence- a roughened area where the superior ramus of the pubic bone meets the ilium
6. Superior ramus of the pubic bone
7. Upper inner border of the body of pubic bone.
8. Upper inner border of the symphysis pubis.
The midwife needs to be familiar with the fixed points on the pelvic brim that are known as its landmarks. The landmarks of the pelvic brim are used to describe the interplay between the fetus and pelvis as a presenting part descends. The landmarks are the fundamental part of the assessment of descent and engagement of the presenting part. It is very important part for the assessment of the progress of pregnancy and labour. The nurse assist the engagement of the presenting part during abdominal and vaginal examination.
Three diameters are measured in the brim:
Anteroposterior diameter.
This diameter extends from the sacral promotory to the upper inner border of the symphysis pubis
and measures approximately 11cms
There are three anteroposterior diameters of the inlet:
1. Conjugata vera: The true conjugate of the inlet; extends from the middle of the sacral promontory to the middle of the upper margin of the symphysis pubis; normally measures 11 cm or more.
2 Obstetric conjugate of the inlet: Extends from the middle of the sacral promontory to the middle of the symphysis pubis on its inner surface a short distance (several millimeters) below its upper margin. The minimum measurement of this diameter before the pelvis is considered contracted is 10 cm. This is the shortest antero-posterior diameter because the symphysis pubis is slightly thicker at this point than at its upper or lower margin.
3. Diagonal conjugate of the inlet: extends from the middle of the sacral promontory to the middle of the inferior (lower) margin of the symphysis pubis. The diagonal conjugate is the only diameter of the pelvic inlet that can be measured clinically. A normal clinical measurement is considered to be at least 11.5 cm.
The transverse diameter of the pelvic inlet measures the greatest distance between the linea terminalis on either side of the pelvis; this distance is approximately 13 cm or a little less, depending on the shape of the pelvis.
The oblique diameters of the pelvic inlet measure the distance between the sacroiliac synchondrosis on one side of the pelvis and the iliopectineal eminence on the opposite side of the pelvis. The sacroiliac synchondrosis on the right or left of the pelvis. determines whether the diameter is the right oblique diameter or the left oblique diameter. For example, if the diameter extends from the right sacroiliac synchondrosis to the left iliopectineal eminence, it is the right oblique diameter. The oblique diameters average 12 cm.
The pelvic cavity
The mid-pelvis (cavity) occupies the space between the inlet and outlet. It is through this snug, curved space that the fetus must travel to reach the outside. As the fetus passes through this small area, its chest is compressed, causing lung fluid and mucus to be expelled. This expulsion removes the space occupying fluid so that air can enter the lungs with the newborn's first breath.
It curves with the sacrum and coccyx, and hence is longer behind than in front. The anterior wall is formed by the pubic bones and symphysis pubis and its depth is 4 cm. The posterior wall formed by the curve of the sacrum, which is 12 cm in length.
The cavity is circular in shape and although it is not possible to measure its diameters exactly, they all are considered to be 12cm.
It is of diamond shape.
The pelvic outlet can be described as two outlets: the anatomical and the obstetrical outlet.
The anatomical outlet is formed by the lower boarders of each of the bones together with the sacrotuberous ligament. It is lozenge-shaped bounded by the lower border of symphysis pubis, pubic arch, ischial tuberosities, sacrotuberous and sacrospinous ligaments and, tip of the coccyx.
Obstetric outlet
The obstetrical outlet is of greater practical significance because it includes the narrow pelvic str the two ischal spines and the lower boarder of the symphysis pubis. The obstetrical outlet is t through which the fetus must pass. The narrow pelvic strait lies between the sacrococcygeal join space between the narrow pelvis start and the anatomical outlet. This outlet is diamond shaped. It a segment, the boundaries of which are the roof is the plane of least pelvic dimension, the floor is t anatomical outlet, anteriorly the lower border of symphysis pubis, posteriorly the coccyx, lateral the ischial spin
Diameters of Pelvic Outlet
Antero posterior diameters:
It is the line from the lower border of symphysis pubis to the sacrococcygeal joint. It measure 13cm. As the coccyx may be deflected backward during second stage of labour, this diamete indicated the space available during delivery
The oblique diameter is said to be between the obturator foramen and the sacrospnous ligament, although there are no fixed points. The measurement is taken as being 12cm.
Transverse diameters is the line between the two ischial spines and measures 10-11 cm. It narrowest diameter in the pelvis.
The diameters of the pelvis and its significance in childbirth:
The major obstetric interest in the female bony pelvis is that it is not distensible, with only ming degrees of movement being possible at the symphysis pubis and sacroiliac joints. The various dimensions of the pelvis are therefore particularly significant in the context of childbirth and the successful passage of Cavity the fetus through the bony pelvic structure. The most common type of female pelvis (gynaecold) is considered Outer to be the optimal shape and size for childbirth; this is providing the fetus isn't above average size and the pelvis isn't smaller than average, or where there is a combination of both factors.
During pregnancy, the elevated levels of oestrogen, progesterone and relaxin play a major role i increasing the laxity of the pelvic girdle joints. The hormonal levels do return to normal in the weeks following childbirth, but the time taken will also be affected by breastfeeding. By 3 to 6 months postnatal, the pelvic girdle should return to its pre-pregnant state; it may need external stabilisation during this period.
An increase has been found in the width of the symphysis pubis from 4 mm to 9 mm in asymptomatic women on X-ray. The separation of less than 1 cm should be considered normal, a greater separation being considered a partial or complete rupture; this may be up to 12 cm. resulting in tension and pain at the sacroiliac joints or symphysis pubis, or both.
In the full squatting position; it has been estimated that the area of the outlet can be increased by as much as 28% in this way. In squatting, the femora apply pressure to the ischial and pubic rami, thus producing separation outward at the symphysis pubis and an upward and backward rotation of the sacrum
The False Pelvis
The false pelvis, which is above that plane, is sometimes considered to be a part of the abdominal cavity, rather than a part of the pelvic cavity The false pelvis has little obstetric significance relevant to the passage of the fetus through the pelvis.
Pelvic Inclination
When the woman is standing in the upright position, her pelvis is on an incline. The anterior superior iliac spines are immediately above the symphysis pubis in the same vertical plane. The brim is tilted and if the line joining the sacral promontary and the top of the symphysis pubis were to be extended, it would from an angle of 60 degree with the horizontal floor. Similarly if the line joining the centre of the sacrum and the centre of symphysis pubis were to be extended, the resulted angle with the floor would be 30 degree. The angle of inclination of the outlet is 15 degree. When the woman is in the recumbent position the same angles are made with the vertical, which should be kept in mind when carrying out an abdominal examination.
Engagement of the Head does not depend only on the size and shape of the brim, but also on the angle of inclination of the brim. The methods of determining this inclination are considered and the angle between the plane of the brim and the front of the body of the 5th lumbar vertebra is found to furnish the best index of the inclination. Analysis of a series of cases shows that this angle varies considerably. Its postural range is demonstrated.
When the inclination is high the head does not easily engage although the measurements may be normal, and a high inclination is one of the commonest causes of unexpected dystocia.
Because these cases are usually selected for a "trial of labour", criteria are necessary to select the cases suitable. Success or failure of trial labour in these cases depends on the amount of room in the upper pelvis. A common type of pelvis causing dystocia is one in which the inclination of the brim is high and the upper sacrum is relatively vertical and convex whereas lower inclination helps in early engagement of the presenting part.
Pelvic Planes
These are imaginary flat surfaces at the brim, cavity and outlet of the pelvic canall at the levels of the lines. A line drawn exactly half-way between the anterior wall and the posterior wall of the pelvic canal would trace a curve called the curve of Carus. The midwife needs to become familiar with the concept in order to make accurate observations on vaginal examination and to facilitate the birth of the baby.
Types of Pelvis and their effect on Birth
In addition to size, the shape of a woman's pelvis is a determining factor for a vaginal birth.
The pelvis is divided into four main shapes: gynecold, anthropoid, android, and platypelloid. The shape of female pelvis is very important from gynecological point of view. The anatomical shape of the female pelvis should be suitable for the passage of baby through it. Otherwise, baby may get stuck inside the pelvis that may make vaginal delivery difficult.
The Gynaecoid Pelvis
The gynecoid pelvis is considered the true female pelvis, occurring in about 50% of all women; is less common in men. Vaginal birth is most favorable with this type of pelvis because the inlet is round and the outlet is roomy, a straight side walls, a shallow cavity with a broad, well curved sacrum blunt ischial spines, a wide sciatic notch and a pubic arch of 90 degree. This shape offers the optimal diameters in all three planes of the pelvis. This type of pelvis allows early and complete fetal internal rotation during labor. So Gynaecoid Pelvis is the most suitable pelvic shape for childbirth.
The Anthropoid Pelvis
The anthropoid pelvis is common in men and occurs in 25% of women. The pelvic inlet is oval and the sacrum is long, producing a deep pelvis (wider front to back [anterior to posterior] than side to side [transverse]. It has larger outlet. The problem in this pelvis is the inlet. The diameters of inlet favor the engagement of fetal head in occiput-posterior position that may slow down the progress of labor If head engages in anterior position then labor progress normally in most of the cases. Vaginal birth is more favorable with this pelvic shape compared to the android or platypelloid shape.
Android Pelvis
The android pelvis is considered the male-shaped pelvis and is characterized by a funnel shape. It occurs in approximately 20% of women. The pelvic inlet is heart shaped and the posterior segments are reduced in all pelvic planes. It has prominent ishial spines and also has narrower transverse outlet diameter. Such pelvis is more likely to be present in tall women. African- Caribbean women are more at risk of having an adroid shaped pelvis. Child birth is difficult and more complicated in android shaped pelvis than gynaecoid pelvis. Women have to push harder, walk more often and chances of instrumental vaginal delivery are high. Descent of the fetal head into the pelvis is slow, and failure of the fetus to rotate is common. The prognosis for labor is poor, subsequently leading to cesarean birth It may prolong the labor.
Platypelloid Pelvis
The platypelloid or flat pelvis is the least common type of pelvic structure among men and women, with an approximate incidence of 5%. The pelvic inlet is specifically kidney shaped brim in which narrow anterio-posterior diameter and the transverse increased.
The pelvic cavity is shallow but widens at the pelvic outlet, making it difficult for the fetus to descend through the mid-pelvis. But platypelloid pelvis don't allow the head to engage with ease, engagement may necessitate lateral tilting of the head, known as asynclitism. But if the head manage to engage then rest of the process of labor may occur normally but in most of the cases it is longer as compared to progress of labor in case of gynaecoid pelvis. Labor prognosis is poor with arrest at the inlet occurring frequently. It is not favorable for a vaginal birth unless the fetal head can pass through the inlet.
Pelvic Floor
The Pelvic floor muscles consists of pubococcygeus, iliococcygeus and ichiococcygeus collectively called levater ani and with the covering fascia is called diaphragm.
The pelvic floor is formed by the soft tissues which fill the outlet of the pelvis. The most important is the strong diaphragm of muscle slung like a hammock from the walls of the pelvis. Through it pass the urethra, the vagina and the anal canal.
Functions
1. Support or act as a "floor" for the abdominal viscera including the rectum, bladder, bowel and uterus in a functional position. Weakness or tear of this sling during parturition is responsible for prolapse of the organs concerned.
2. Assists the closure of the bladder and bowel outlet constrictor or continence mechanism to the urethral, anal and vaginal orifices (in females).
3. It helps maintain optimal intra-abdominal pressure
4. Facilitates anterior internal rotation of the presenting part when it presses on the pelvic floor.
5. Ischiococcygeus helps to stabilize the sacroiliac and sacrococcygeal joints.
6. During childbirth it influences the passive movements of the fetus through the birth canal and relaxes to allow its exit from the pelvis.
Pelvic floor is made up of a number of muscles, which are further organized in superficial and deep parts.
The Superficial Pelvic Floor Muscles
Even though controversy exists as regarding the nomenclature, the superficial muscles include five muscles, external anal sphincter, bulbospongiosus muscle, ischiocavernosus muscle, membranous sphincter of the urethra and transverse perineal muscles. Caudal extension of the circular layer of smooth muscle of rectum into anal canal forms the internal anal sphincter (IAS) and the extension of longitudinal layer of smooth muscle of rectum forms the external anal sphincter (EAS) of the anal canal which is attached behind by a few fibres to the coccyx.
The transverse perineal muscles pass from the ischial tuberosities to the centre of the perineum.
The bulbospongiosus muscle, also called bulbocavernosus muscle, a muscle of the perineum, the area between the anus and the genitals. The bulbospongiosus is located in the middle line of the perineum, in front of the anus. It consists of two symmetrical parts, united along the median line by a tendinous raphé. It arises from the central tendinous point of the perineum and from the median raphé in front.
The ischiocavernosus muscle is a muscle just below the surface of the perineum, It arises by tendinous and fleshy fibers from the inner surface of the tuberosity of the ischium, and from the rami of the pubis and ischium on either side of the crus.
The membranous sphincter of the urethra not a true sphincter as it is not circular but it acts as to close the urethra. It composed of the muscles fibres passing above and below the urethra and attached to the pubic bones.
The deep pelvic floor muscles composed of three pairs of muscles which together are known as the levator ani muscles. The deep pelvic floor muscles (anatomic pelvic floor) include four major muscles namely pubococcygeus, ileococcygeus, ischiococcygeus and puborectalis.
The pubococcygeous muscle passes from the pubis to the coccyx, with a few fibres crossing over in the perineal body to form its deepest part.
The illococcygeus muscles passes from the fascia covering the obturator internus muscles (the white line of the pelvic fascia) to the coccyx.
The ichiococcygeus muscle passes from the ischial spine to the coccyx, in front of the fibers which form a sling for the rectum are named the Puborectalis. They arise from the lower part of the pubic symphysis, and from the diaphragm. They meet with the corresponding fibers of the opposite side around the lower part of the rectum, and form for it a strong sling. Relaxation increases the angle between rectum and anus, allowing defecation in conjunction with relaxation of the internal and external anal sphincters.
Between the muscles layers, and also above and below them, there are layers of pelvic fascia. This is loose areolar tissue which is used like packing material space in between the bulbocavernosus, the ischiocavernosus and transverse perineal muscles is known as triangular ligament.
The Perineal Body
The perineal body is an irregular and fibromuscular mass. It is located at the junction of the urogenital and anal triangles-the central point of the perineum. This structure contains skeletal muscle, smooth muscle and collagenous and elastic fibres.
Anatomically, the perineal body lies just deep to the skin. It functions as a point of attachment for muscle fibres from the pelvic floor and the perineum itself:
- Levator ani (part of the pelvic floor).
- Bulbospongiosus muscle.
- Superficial and deep transverse perineal muscles.
- External anal sphincter muscle.
- External urethral sphincter muscle fibres.
Prevention of the Perineal Floor from injury during Child Birth
- In women, it acts as a tear resistant body between the vagina and the external anal sphincter, supporting the posterior part of the vaginal wall against prolapse. It also supports the anterior vaginal wall, bladder and the uterus.
- Childbirth can lead to damage (stretching/tearing) of the perineal body, thus leading to possible prolapse of pelvic viscera. This may be avoided by an episiotomy (a surgical cut in the perineum) This inevitably causes damage to the vaginal mucosa, but prevents uncontrolled tearing of the perineal body.
- The delivery of the head should be done between contractions. The early extension of the head must be avoided during delivery of the head.
- Waterbirth and labouring in water are popular for several reasons, and it has been suggested that by softening the perineum they might reduce the rate of tearing. However, this effect has never been clearly demonstrated.
- Antenatal digital perineal massage is often advocated, and may reduce the risk of trauma only in nulliparous women.
The Perineum
The perineum is a diamond-shaped area between the buttocks and thighs lies below the pelvic floor. It is divided into an anterior urogenital triangle that contains the external genitalia and a posterior anal triangle that contains the anus.
The urogenital triangle is the anterior part of the perineum. In female mammals, it contains the vagina and associated parts of the external genitalia. The urogenital triangle is the area bound by a triangle with one vertex at the pubic symphysis and the two other vertices at the ischial tuberosities of the pelvic bone. It is bounded by the pubic symphysis, ischiopubic rami, and an imaginary line between the two ischial tuberosities. The triangle is associated with the structures of the urogenital system - the external genitalia and urethra.
Structurally, the urogenital triangle is complex, with a number of fascial layers and pouches. Unlike the anal triangle, the urogenital triangle has an additional layer of strong deep fascia, known as the perineal membrane. This membrane has pouches on its superior and inferior surfaces. The layer of the urogenital triangle are (deep to superficial)
Deep perineal pouch: A potential space between the pelvic floor superiorly, and the perineal membrane inferiorly. It contains part of the urethra and the external urethral sphincter. In males, it also contains the bulbourethral glands and the deep transverse perineal muscles.
Perineal membrane: A layer of tough fascia, which is perforated by the urethra and vagina. The role of the membrane is to provide attachment for the muscles of the superficial external genitalia, and to help support the pelvic viscera.
Superficial perineal pouch: A potential space between the perineal membrane superiorly, and the perineal fascia inferiorly. It contains the erectile tissues that form the penis and clitoris, and three muscles the ischiocavernosus, bulbospongiosus and superficial transverse perineal muscles. The greater vestibular glands (Bartholin's glands) are also located in the superficial perineal pouch.
Deep perineal fascia: Fascia covering the superficial perineal muscles.
Superficial perineal fascia: It is continuous with the superficial fascia of the abdominal wall. The superficial fascia itself can be divided into superficial and deep layers. The superficial layer is fatty in structure, forming the labia majora and mons pubis in women.
Skin-The urethral and vaginal orifices open out onto the skin.
Anal Triangle
The anal triangle is the posterior part of the perineum. It contains the anal canal. The anal triangle can be defined either by its vertices or its sides.
Vertices
- One vertex at the coccyx bone
- The two ischial tuberosities of the pelvic bone
Sides
- Perineal membrane (posterior border of perineal membrane forms anterior border of
- The two sacrotuberous ligaments
Contents of Anal Sphincter are:
- Ischioanal fossa
- Anococcygeal body
- Internal pudendal artery and Internal pudendal vein
- Sacrospinous ligamen
- Anal canal
- Sacrotuberous ligament Pudendal nerve
Muscles
- Sphincter ani externus muscle
- Obturator internus muscle
- Coccygeus muscle
- Gluteus maximus muscle
- Levator ani muscle
Pelvic Floor Exercise
A woman's pelvic floor muscles support her bladder, womb (uterus) and bowel (colon). The urine tube (front passage), the vagina and the back passage all pass through the pelvic floor muscles. The pelvic floor muscles help to control bladder and bowel. They also help sexual function. It is vital to keep your pelvic floor muscles strong. Pelvic floor muscles can be made weaker by:
- not keeping them active
- being pregnant and having babies
- constipation
- being overweight
- heavy lifting
- coughing that goes on for a long time (such as smoker's cough, bronchitis or asthma); and
- old age
Procedure
- Squeeze and draw in the muscles around back passage and vagina at the same time. Lift them Up inside. The client should have a sense of "lift" each time squeeze pelvic floor muscles. Try to hold them strong and tight and count to 8. Now, let them go and relax.
- Repeat "squeeze and lift" and let go. It is best to rest for about 8 seconds in between each lift up of the muscles or hold for as long as she can.
- Repeat this "squeeze and lift" as many times as she can, up to a limit of 8 to 12 squeezes.
- Try to do three sets of 8 to 12 squeezes each, with a rest in between.
- Do this whole training plan (three sets of 8 to 12 squeezes) each day while lying down, sitting or standing.
While doing pelvic floor muscle training:
- keep breathing:
- do NOT tighten your buttocks; and
- only squeeze and lift;
- keep thighs relaxed.
HUMAN SEXUALITYonly squeeze and lift;
Human sexuality is the way in which we experience and express ourselves as sexual beings (Rathus et al., 1993). There are many factors that help develop our sexuality, arguably one of the most important. is our actual gender. Whether, one is a male or female will likely have a major influence on the development of individual sexuality. Furthermore, sexuality is an integral part of our personalities whether we are aware of it or not.
Human sexual behavior is different from the sexual behavior of other animals, in that, it seems to be governed by a variety and interplay of different factors. That is, while "lower" animals or species are driven by a "force" to reproduce and therefore partake in sexual behavior. Humans are not sexually active just for the sake of reproduction, rather, there are a variety of complex factors that lead people to have sex.
It is determined by anatomy, physiology, psychology, culture, relationship with others, and developmental experiences
Sexual intercourse, also called coitus, or copulation, is the reproductive act in which the male penis enters the female vagina. If the reproductive act is complete, an average of 100 million sperm are ejaculated from the male body into the female.
The menstrual cycle is hormonally driven, and can be divided into approximately two halves: In the follicular phase, secretions of luteinizing hormone, follicle-stimulating hormone, and estrogen support the growth of the follicle (the cell complex that surrounds and nurtures the egg) in the ovary and build up the lining of the uterus to receive a fertilized egg
The average woman has a 28 day fertility cycle. Day 1 is assigned to the first day of her menstrual period. That menstrual cycle lasts an average of 5 days. From day 6-12 or 13, a new egg is maturing inside an ovarian follicle, and a new lining is forming inside the uterus in preparation for a fertilized egg On day 14 or so, the mature egg erupts from the follicle and is swept up and into the fallopian tube. Any sperm that were already present in the tube or that newly enter the tube may fertilize the egg during the next 24 hours.
If the egg is not fertilized, it dissolves and the uterine lining continues to thicken. If the egg is fertilized, it implants itself in the uterine lining. The empty follicle, filled with corpus luteum, now produces large amounts of progesterone to signal the body that a pregnancy is proceeding At mid-cycle, when the egg is ready, a surge of LH and FSH chemically signals the ovary to release the
egg. This stage is called ovulation, and is the optimum time for fertilization to take place.
In the luteal phase, the remnants of the follicle (corpus luteum) keep secreting estrogen and progesterone to maintain the readiness of the uterus. If the egg is fertilized, then the luteal phase continues throughout pregnancy. If the egg is not fertilized, then the corpus luteum dies, the uterus sheds its lining, menses begins.
Each month inside the woman's ovaries, a group of eggs starts to grow in small, fluid-filled sacs called follicles. Eventually one of the eggs erupts from the follicle (ovulation). It usually happens about two weeks before the next period.
After the egg leaves the follicle, the follicle develops into the corpus luteum. The corpus luteum
releases a hormone that helps thicken the lining of the uterus, getting it ready for the egg
HUMAN CONCEPTION
Gametogenesis
Primordial Germ Cells
Development begins with fertilization, the process by which the male gamete, the sperm and the female gamete, the oocyte, unite to give rise to a zygote. Gametes are derived from primordial germ cells(PGCs) that are formed in the epiblast during the second week and that move to the wall of the yolk sac. During the fourth week, these cells begin to migrate from the yolk sac toward the developing gonads, where they arrive by the end of the fifth week. Mitotic divisions increase their number during their migration and also when they arrive in the gonad. In preparation for fertilization, germ cells undergo gametogenesis, which includes meiosis, to reduce the number of chromosomes and cytodifferentiation to complete their maturation.
Spermatogenesis
It is the process of maturation of male gametes in the wall of seminiferous tubules and starts at puberty but when does it stops is not known because it is extremely variable. It includes series of cyclical changes for the conversion of the primordial male germ cells into spermatozoa. Spermatogenesis consists of three stages:
1. Spermatocytosis
2. Meiosis
3. Spermiogenesis
1. Spermatocytosis
The primordial germ cells divided by mitosis and form dark type A spermatogonia which act as the stem cells. Each dark type A cell gives rise to two daughter cells by mitosis, one dark type A spermatogonium and the other light type A spermatogonium. The dark type A cell is kept as a reserve for the repetition of the next cycle. The light type A cell is more differentiated and undergoes mitotic division to form two type B spermatogonia. Mitosis extends to produce about four generations of type B cells. Each type B cell further divides into two primary spermatocytes each of which possesses 46 chromosomes (44 autosomes XY sex chromosomes).
2. Meiosis
Hence forward, first meiotic or reduction division affects each primary spermatocyte and yields two daughter cells, the secondary spermatocytes. The secondary spermatocytes, each containing 23 chromosomes (haploid), consist of two varieties-one with 22 autosomes plus X chromosome and the other with 22 autosome plus Y chromosome. Unlike the oocyte, however, both secondary spermatocytes contain equal amount of cytoplasm and are equally active. The secondary spermatocytes almost immediately complete the second meiotic division, resulting in the formation of the spermatids. Therefore, each primary spermatocyte yields four spermatids, two of them are X-bearer and the remaining two Y-bearer. The spermatids are then metamorphosed into spermatozoa. In both spermatogenesis and oogenesis each daughter cell of the first meiotic division possesses haploid chromosomes with 2N DNA strands, whereas each daughter cell of the second meiotic division contains haploid chromosomes with 1N DNA strand because DNA replication does not take place in meiosis II.
3. Spermiogenesis
Morphological transformation of spermatids into spermatozoa without further cell division, is termed the spermatogenesis. Initially each spermatid possesses a spherical nucleus, Golgi apparatus, a centrosome with two centrioles, numerous mitochondria and abundant cytoplasm.
As the conversion progresses, the flattened vesicles of Golgi apparatus containing acrosomal granules coalesce and spread over the anterior pole of the nucleus forming the head cap. The head cap covers two-third of the nucleus. The centrosome occupies the posterior pole of the nucleus opposite to the head cap, and splits into two centrioles which give rise to axial filaments of the body and tail of a spermatozoon. The two centrioles delimit the middle piece or body of the spermatozoon; the posterior one forms the ring centriole. Around the middle piece, all the mitochondria are aggregated in a spiral manner and form the mitochondrial sheath. Finally, the spermatid elongates and the nucleus is evaginated from the cytoplasm but remains within the cell membrane, constituting the head of the spermatozoon. Some amount of cytoplasm surrounds the body or the middle piece, but most of the cytoplasm content is extruded from the cell as residual bodies.
The heads of the immature spermatozoa plunge into depressions at the surface of the cells of Sertoli. When maturity is reached, they are set free into the lumen of the seminiferous tubules. The whole process of conversion from the type A spermatogonia to the spermatozoa requires approximately 64 days in man. Spermatocytosis requires about 16 days, Meiosis 1-8 days, Meiosis 11-16 days and spermatogenesis about 24 days.
Fully formed spermatozoa in the seminiferrous tubules are non-motile and reach the epididymis by suction action. The mucous membrane of the rete testes, efferent ductules and proximal part of the canal of epididymis reabsorb the fluid product of the testis. As a result a negative pressure is created in the epididymis, and this helps in transport of the spermatozoa from the seminiferous tubules to the epididymis.
Oogenesis
This is a process of maturation of primordial female germ cells, from primary oocyte to matur ovum. Maturation is affected by a process of meiosis, which consists of two consecutive divisions Meiosis I is a heterotypical or reduction division, and Meiosis II is a homotypical division of already reduced first one. Associated with the maturation of germ cells, a number of primary follicles, about 5-12 follicles, mature after puberty in each monthly menstrual cycle. As a rule, only one follicle matures fully and ruptures in each month, shedding the oocytes from the surface of ovary. Rest of the follicles undergo atretic changes.
Process of Maturation
A primary ovarian follicle consists of a central large cell known as the primary oocyte, which is surrounded by a layer of flattened follicular cells. The primary oocyte, which already completes the
the prophase of first meiotic division, is initially about 35 microns in diameter. The nucleus of the oocyte is eccentric in position and contains diploid number of chromosomes with 44 autosomes and 2x sex chromosomes.
As the follicle undergoes maturation, the primary oocyte enlarges and reaches a diameter of about 140 microns. The follicular cells become cuboidal and multiply into several layers of cells
. Meanwhile, scattered amorphous materials rich in glycoprotein accumulate between the inner layer of follicular cells and oocyte. These substances fuse and form a complete striated membrane known as the zona pellucid around the oocyte. The zona pellucid may be derived from the follicular cells or the oocyte or from both.
Numerous microvilli of the primary oocyte project into the processes from the follicular cells. These processes make the zona striated in appearance and help to convey nutrition to the oocyte. As the follicle enlarges, numerous fluid filled spaces appear in between the follicular cells. These spaces coalesce to form a single cavity known as the antrum folliculi and the fluid is called liquor folliculi
As a result, the follicular cells separate into an outer layer named as the inner layer called the cumulus overicus, but both layers are continuous at one place. The cumulus surrounds the primary oocyte. Outside the stratum granulosum of the follicle, stroma cells of the ovary are organized to form a sheath known as the theca folliculi, which differentiates into two layers; an inner vascular and cellular layer, the tunica interna and an outer fibrous layer, the tunica externa.
A basement membrane intervenes between the cells of the interna and stratum granulosum. At this stage the primary oocyte from the dictyotene stage completes the first meiotic division which was started during prenatal life. The nuclear membrane disappears and the chromosomes arrange themselves in homologous pairs at the equator of the achromatic spindle. The spindle is situated eccentrically close to one pole of the oocyte. After the cross-over, the chromosomes separate and one member of each pair passes centrally, while the other member passes outwards and separates from the oocyte to form the first polar body.
The result of this division is the formation of the two daughter cells, each with 23 chromosomes the cytoplasmic division is unequal. One cell is large, receives abundant cytoplasm of the mother cell (haploid number, 22 autosomes and one X chromosomes). Although the nuclear division is equal, and is known as the secondary oocyte. The other cell is small carrying scanty amount of cytoplasm and persists as the first polar body. The polar body is accommodated in the perivitelline space which has meanwhile appeared between the zona pellucid and the cell membrane of the secondary oocyte
A mature follicle containing secondary oocyte and first polar body is known as the Graafian follicle. The secondary oocyte immediately enters in the process of second meiotic division. The haploid chromosomes rearrange themselves at the equator of the spindle which occupies close to one pole to the cell.
The Graffian follicle fully matures, assumes a size of about 10 mm and appears immediately beneath the surface of the ovary.
Things to remember
Questions and Answers
Explain the management of male infertility?
Management of Male Infertility
General Measures
- Examples of sexual counseling education include teaching about coitus frequency and timing during a fertile period, coitus posture, and avoiding masturbation because it dilutes sperm.
- Overall health improvement, including weight loss in obese patients.
- Avoid excessive drinking and smoking.
- Avoid wearing tight-fitting or hot underwear, and wash your scrotum for five minutes in cold water at least twice daily.
- Overly frequent abstinence from intercourse may boost sperm production.
- Avoid strenuous exertion, jobs outside in the sun, etc.
- Repair of thyroid and diabetic issues without delay
- The use of vitamin E, C, B12, and folic acid also helps to promote spermatogenesis and the harmful free radicals that are generated by damaged sperm and leukocytes found in the semen.
Treatment of Genital Tract Infection
- Using the appropriate antibiotics to treat epididymo-orchitis, prostatitis, and sexually transmitted diseases.
Management of Hypogonadotropic-Hypogonadism (Endocrinal Correction)
With varying degrees of success, the following therapies can be used to treat spermatogenesis disorders.
- Clomiphene citrate for reduced or low gonadotrophins
- Once or twice a week, intramuscular injections of HCG (5000 IU) are given to boost the production of endogenous testosterone.
- HMG or HCG are used when clomiphene citrate therapy has failed or when there is a gonadotrophin deficit.
- To treat hypothalamic dysfunction, a minipump is used to administer GnRH infusions.
- Bromocriptine is used to treat hyperprolactinemia.
In Retrograde Ejaculation
- Phenyl ephrine can enhance the tone of an internal urethral sphincter.
- If a guy has anti-sperm antibodies, dexamethasone 0.5 mg once a day at bedtime may be beneficial.
Artificial Insemination of Husband
- In artificial insemination by husband (AIH), a sperm sample from the woman's partner is inserted into the uterus (the womb) using a tiny catheter (tube) through the cervix, the natural opening of the uterus. The goal of this treatment is to promote fertilization and pregnancy. AIH is different from artificial insemination by donor (AID), in which the donor is a man other than the woman's mate. AIH also falls under the definition of "homologous insemination."
Surgical Management
- The two treatments for vas deference blockage are epididymectomy and vaso-vaso anastomosis.
- Surgery is used to repair the hydrocele, and high spermatic vein ligation is used to treat varicocelo if it is present.
- To ensure adequate spermatogenesis in later life, orchidopexy should be performed on undescended testes between the ages of two and three.
- Use of methods for assisted reproduction
© 2021 Saralmind. All Rights Reserved.



 Login with google
Login with google