ORGAN FUNCTION TEST
Subject: Basic Science Applied to Nursing

Overview
Liver Functions Test (LFT)
LFT Profile
The term "LFT profile" refers to a collection of regular laboratory tests used to assess liver functioning. Under the LFT profile, several biochemical studies are conducted to assist identify the
the degree of anomalies and liver damage.
LFT profile include the following parameters:
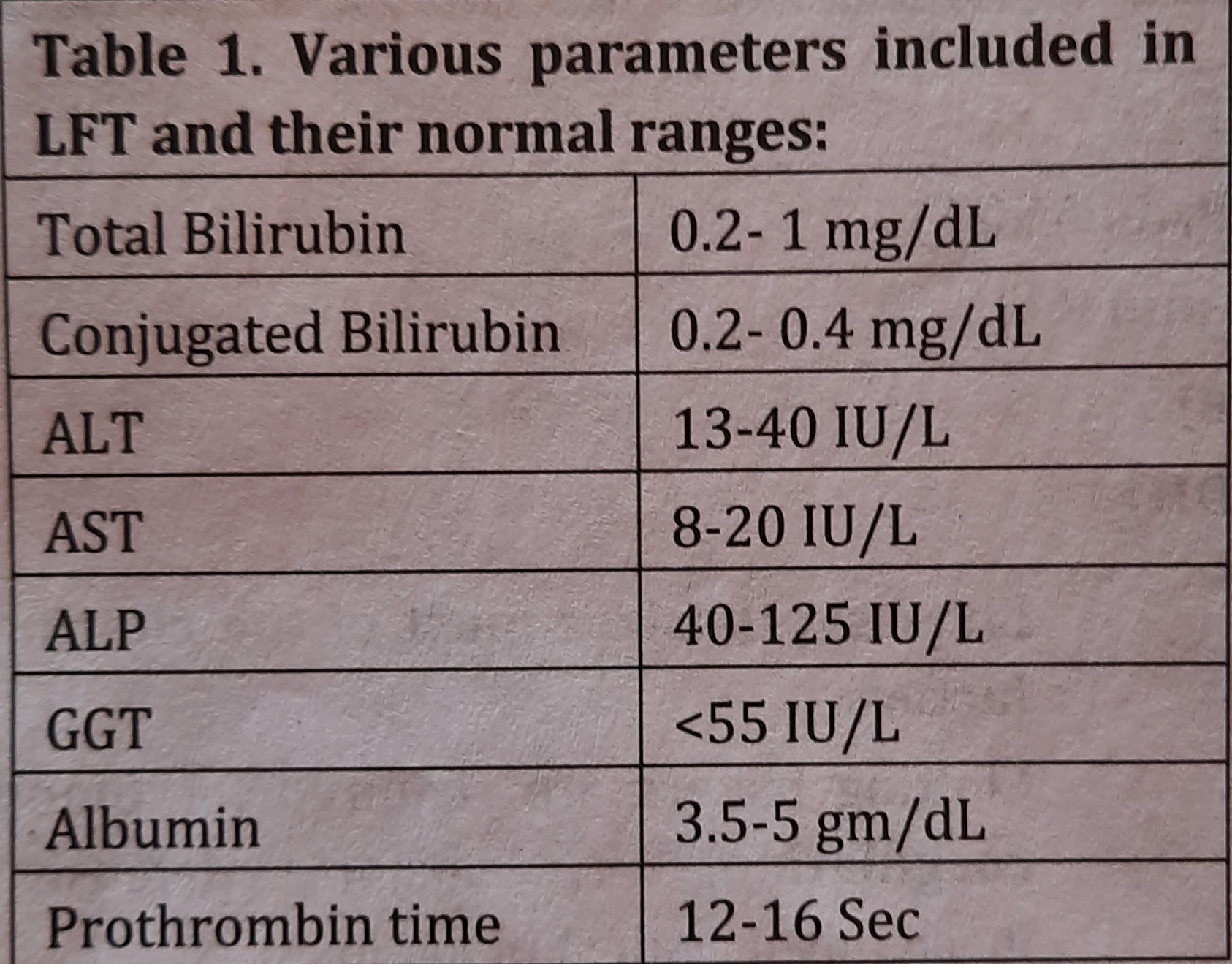
[ALT= Alanine Amino Transferase; AST = Aspa Amino Transferase; ALP- Alkaline Phosphatase; GGT=Gamma Glutamyl Transferase]
Indications of LFTs:
Liver function tests are helpful in
- differential diagnosis of jaundice
- detecting liver abnormalities
- detecting extent and type of liver damage
Liver Function Tests classification:
Major liver function tests or LFT profile may be classified on various bases:
- Tests based on excretory functions of liver: Total and conjugated bilirubin is estimated in serum.
- Tests based on serum enzymes profile: Activity of various enzymes, such as ALT, AST, ALP, GGT and 5'-nucleotidase (5'NT) are estimated in serum.
- Tests based on synthetic function:
- Serum albumin
- Prothrombin time (PT)
1. Tests based on excretory functions of liver:
Total and conjugated bilirubin are estimated in serum.
Bilirubin:
- The excretory byproduct of heme breakdown is bilirubin. It is mostly made when hemoglobin (Hb) breaks down, with some help from myoglobin and other hemoproteins.
- This unconjugated (water-insoluble) bilirubin is delivered to the liver by albumin in the circulation.
- Glucuronyl transferase in the liver converts unconjugated bilirubin to conjugate form. Water soluble conjugated bilirubin (bilirubin diglucuronide) is produced in this way and can be eliminated through the bile duct, the intestine, and eventually the feces and urine.
Normal range of bilirubin:
Normal range of bilirubin in serum or blood is as follows
- total bilirubin: 3.2 - mg / d * L and
- conjugated bilirubin: 0.2-0.4 mg/dL.
When the bilirubin level exceeds 1 mg/dL, it is hyperbilirubinemia. known as
Hyperbilirubinemia may be due to:
- generation of bilirubin in excess of what the liver can conjugate and eliminate,
- damaged liver that is unable to eliminate bilirubin even when generated in normal levels,
- occlusion of the liver's excretory ducts, which prevents bilirubin from being excreted,
[Note: Bilirubin 22.5 mg/dL in blood is called as jaundice or icterus.]
Jaundice
The word jaundice is derived from French word, Jaune means yellow. Jaundice is defined as yellowish coloration of skin and sclera due to diffusion of bilirubin from blood to the tissues.
It occurs when bilirubin in serum is greater than 2.5mg / d * L
Jaundice is most commonly classified on the basis of site of disorder:
- Prehepatic (hemolytic) jaundice
- Hepatic (hepatocellular) jaundice
- Posthepatic (obstructive) jaundice
Prehepatic Jaundice:
- It is caused by excessive hemolysis, which is the breakdown of RBCs and hemoglobin, meaning that the more RBCs are broken down, the more bilirubin is produced.
- Hemolytic anemia, thalassemia, incompatible blood transfusions, etc. all cause prehepatic jaundice.
Feature:
- Unconjugated hyperbilirubinemia (↑↑ed unconjugated bilirubin in blood).
Hepatic Jaundice:
- It is due to liver disease. It may be due to virus infection (viral hepatitis), alcohol (alcoholic liver disease or liver cirrhosis), or due to genetic cause (due to defect in conjugating enzyme).
Features:
- Bilirubin: biphasic hyperbilirubinemia (ted unconjugated and conjugated bilirubin in blood).
- Enzymes: Serum ALT and AST are raised. In most type of liver disease ALT activity is higher than that of AST activity. In case of intrahepatic obstruction, ALP activity is also raised.
Posthepatic Jaundice:
- It is due to obstruction in biliary tract. Obstruction leads to an accumulation of bilirubin in bile duct, causing irritation of the biliary cells resulting into release of ALP, 5'-NT or GGT from these cells into the blood.
Features:
- Bilirubin: Conjugated hyperbilirubinema (††ed conjugated bilirubin in blood).
- Enzymes: Serum ALP and 5'-NT GGT are raised significantly.
Tests based on serum enzymes profile
Following enzymes- ALT, AST, ALP and GGT are estimated to assess LFT. Raised levels of these enzymes occur in hepatic or post hepatic disease.
- Aminotransferases:
- Alanine aminotransferase (ALT or SGPT)
- Aspartate aminotransferase (AST or SGOT)
These enzymes typically reside inside hepatic cells, and the serum (plasma or blood) levels of these substances are relatively low (10–40 IU/L).
However, the release of these enzymes into the plasma may result from the loss of hepatic cells (from any kind of hepatitis).
Acute hepatocyte injury or hepatitis are indicated by elevated levels of these enzymes in plasma. Hepatic jaundice appears in this scenario.
- Alkaline Phosphatase (ALP):
- This enzyme is present on hepatobiliary cells and on the cells of on bile canaliculi. During obstruction of biliary duct (by cholestasis, or by tumor of head of pancreas), ALP is released in plasma.
- Hence, increased level of ALP in plasma indicates obstructive or post hepatic disease or jaundice.
- Gamma Glutamyl Transferase (GGT):
- This enzyme can be activated. Alcoholism and drug addiction increase the amount of this compound since these substances stimulate the liver's production of it (phenytoin, phenobarbitone, etc.).
- Therefore, measuring the activity of this enzyme is crucial for identifying alcohol and drug misuse.
- Post-hepatic jaundice is indicated by plasma GGT levels that are markedly elevated.
- [GGT is elevated in drug and alcohol addicts, as well as in cases of hepatobiliary blockage]
Tests based on synthetic function
Albumin:
This is the major protein in plasma which is exclusively synthesized by liver. The half life of albumin in plasma is approximately 20 days.
So, in case of liver disease (of more than 20 days), the levels of albumin in plasma is decreased. Normal range of albumin in plasma: 3.5 5gm/dL.
- If level of albumin falls below 2.5 gm%, it indicates liver is unable to synthesize albumin i.e. liver disease.
- Decreased levels of albumin in plasma indicates the chronicity of liver disease.
Prothrombin time (PT):
- One of the clotting factors produced by the liver is thrombin. Prothrombin synthesis is reduced in liver illness. As a result, PT is a helpful measure of liver health.
- Prothrombin in plasma has a 6-hour half-life. Blood clotting takes longer in cases of acute liver disease. It denotes an increased or extended prothrombin time (PT). 12 to 16 seconds constitute a typical PT.
Renal Function Tests
Renal Function Tests (RFT) or Kidney Function Tests (KFT) are done to assess the normal functioning of Kidneys as well as to detect the extent and types of kidney diseases.
Purpose of RFT
- To assess functional capacity of kidneys
- Early detection of possible renal impairment
-
Monitor the response to treatment of renal diseases
Indications of RFT
- a history of chronic renal disease in the family
- sweet diabetes
- Hypertension
- infections of the urinary tract (UTI)
- Nephrolithiasis Lower urinary tract blockage
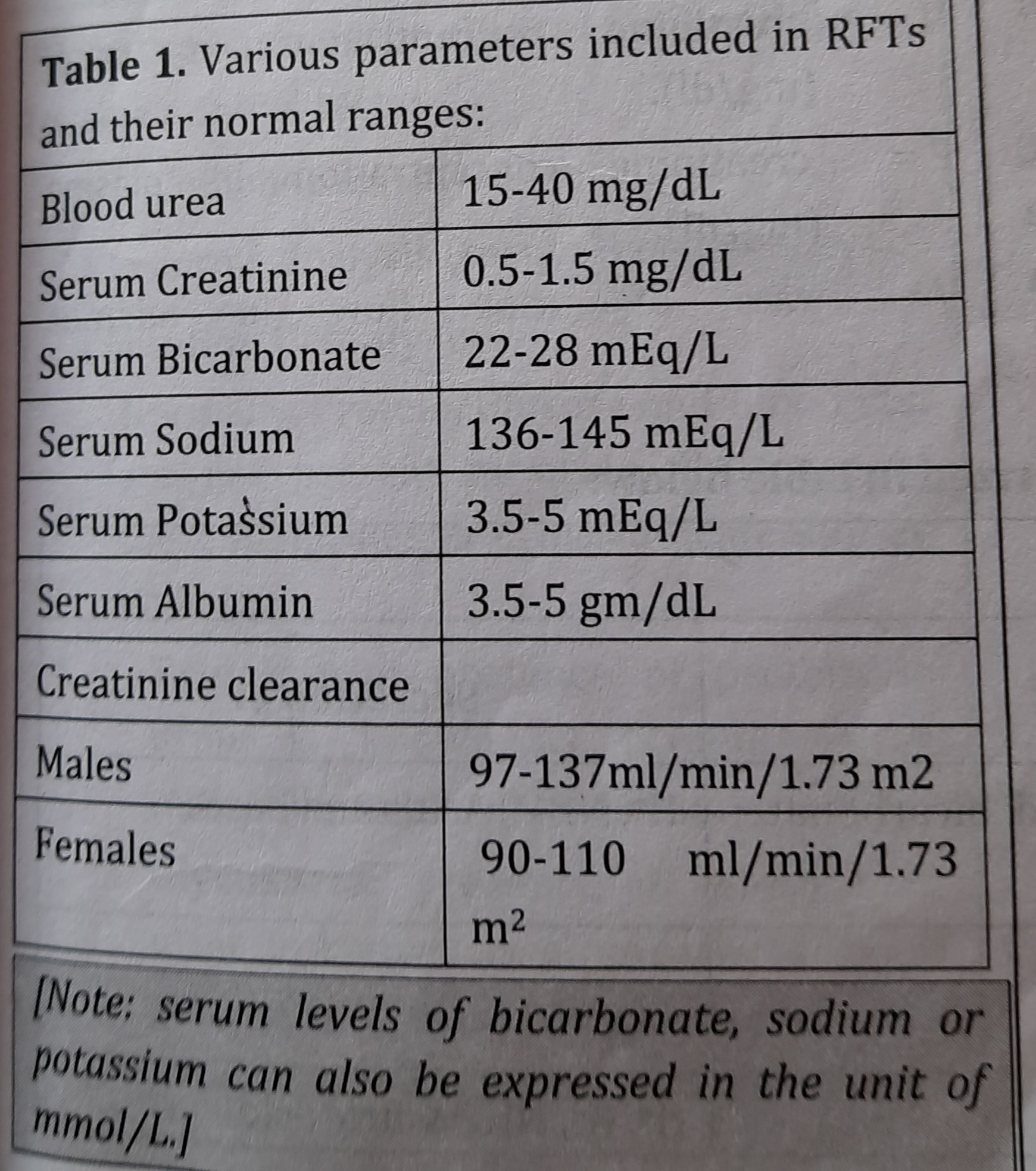
RFT Profile:
RFT profile refers to a group of tests routinely done in the laboratory to evaluate renal functions.
A number of biochemical investigations are done under RFT that will help detect the abnormalities of the kidney function.
RFTs will provide results in following parameters/analytes.
Classification of RFT
Glomerular Functions:
Glomerular Filtration Rate (GFR)
The glomerular filtrate is an ultrafiltrate that is created on the glomerulus as a result of blood perfusion through Bowman's capsule.
An adult person's GFR is 120–125 ml per minute.
Only 1.5 to 2.5 liters of the glomerular filtrate, which is produced in amounts of 170-180 liters per day, is eliminated as urine. This indicates that the majority of the water in glomerular filtrate is reabsorbed.
GFR in an adult person is 120–125 ml/min (about 170-180 L/day).
Glomerular Permeability
All blood constituents, with the exception of blood cells (Red Blood Cells, or RBCs) and proteins, are filtered by the glomerular membrane (Albumin).
Albumin (molecular weight 69 kDa) and other bigger proteins cannot pass through the glomerular membrane's sieves and are instead trapped in the blood. Therefore, the presence of albumin in urine is the first indication of impaired glomerular function.
It signifies that the presence of blood cells or proteins in urine is a sign of injury to the kidneys' glomerular membranes. Proteins and blood are excreted in the urine, much as they are in cases of nephropathy or glomerular nephritis.
- Glomerular functions include the urea, creatinine and inulin clearance test.
- If kidney function is normal, the waste products in the blood such as urea, creatinine, etc. are normally filtered through glomerular membrane and are excreted through urine.
- However, if kidney function is impaired/abnormal, the waste products cannot be excreted leading to their raised levels in the blood.
Tubular functions:
- The correct reabsorption of analytes from the renal tubular lumen or the discharge of analytes into the tubular lumen are examples of tubular functions. For instance, the tubular cells may reabsorb glucose, amino acids, water, Na, K, and Cl- from the lumen. Similar to this, tubular cells secrete acids (H or NH4), uric acid, and K into the tubular lumen.
However, in cases of aberrant tubular activity, substances such as glucose, amino acids, and others may not be reabsorbed from the tubular lumen, causing their expulsion in urine.
Glycosuria and amino aciduria are the terms used to describe the excretion of glucose and amino acids in urine, respectively.
Clearance Tests
Creatinine Clearance (CC):
GFR is measured via clearance. The amount of plasma that the kidneys totally clear of creatinine in a minute is known as creatinine clearance. Because approximately all of the creatinine that is filtered by the glomerular membrane is eliminated in the urine, creatinine clearance is a superior test for determining glomerular function.
More creatinine in the blood due to decreased creatinine clearance is a sign of glomerular injury (renal damage).
The equation: gives the creatinine clearance (CC):
CC = (UxVx * 1.73)/(PxBodySurfaceArea)
Where,
U = creatinine concentration in urine (mg / dl)
P = creatinine concentration in plasma (mg/dL)
V= rate of urine flow in ml/min.
On the basis of the clinical applications:
- Complete urinalysis
- Serum analysis (serum Biochemistry)
Complete Urinalysis
Normally, Protein, Glucose and Blood etc. are not present in urine. Presence of these molecules in urine indicate kidney damage.
- Proteinuria: presence of protein in urine is known as proteinuria. It indicates glomerular disease.
- Glycosuria: presence of glucose in urine is known as glycosuria. If blood glucose is normal but glucose appears in urine, it is known as renal glycosuria.
- suggests tubular disease (chronic renal failure).
- Hematuria: presence of blood in urine is known as hematuria. It may indicate glomerular nephritis.
Serum Analysis:
- Blood Urea: In normal physiological condition, if blood urea level is greater than normal it is termed as hyperuremia. Hyperuremia indicates glomerular damage.
- Serum Creatinine: Serum creatinine is considered better marker for evaluation of renal function. If level of creatinine in serum is greater than normal (hypercreatininemia), it indicates glomerular damage.
- Sodium (Na): After filtration from glomerular membrane, Na is reabsorbed from different parts of the renal tubule.
- In case of renal tubular disease, blood levels of Nat is decreased (hyponatremia).
- Hyponatremia may cause nausea, weakness, mental confusion or even mental impairment.
Causes of Hyponatremia:
- renal failure, elevated antidiuretic hormone production, and decreased water excretion.
- Spironolactone usage, aldosterone deficit, and other factors can cause salt loss in the urine.
Serum Potassium (K): It is filtered through the glomerular membrane as well as secreted from the tubular cells to the renal tubular lumen..
- In case of renal tubular disease, blood levels of K ^ + is high (hyperkalemia).
Hyperkalemia suggests decreased ability of the kidneys to excrete K+.
Causes of Hyperkalemia:
- Obstructive nephropathy
- Diuretics (spironolactone, amiloride)
- Metabolic acidosis
- Dehydration
Pancreatic Function Test
Indications:
- Diabetes mellitus
- Pancreatic calcification
- Steatorrhoea
Pancreatic Functions Test Profile
Various enzyme are estimated to assess pancreatic function tests. Commonly estimated enzymes to diagnose pancreatic diseases are:
- Serum Amylase
- Serum Lipase
- Trypsinogen
Serum Amylase (AMS) Activity
Normal: 28-100 IU / L
Function: It hydrolyses glycosidic bond of carbohydrates (starch and glycogen) to form oligosaccharides.
Optimum pH for its action: approx 7
Tissue sources of Amylase
- Pancreatic acinar cells and salivary glands are the sources of amylase.
-Pancreatic acinar cells contain p-type amylase
-Salivary glands contain s-type amylase
- Both the types of amylase are present in blood or plasma or serum and may be normally excreted in urine.
Diagnostic significances of Amylase
- The majority of the amylase in blood comes from the pancreas, with a smaller amount coming from the parotid (salivary) gland.
- The most common method of determining amylase levels in blood samples is used to diagnose parotitis and pancreatitis.
- Hyperamylasemia, a condition where very high levels of amylase are released into the blood as a result of pancreatic diseases or obstruction of the pancreatic duct.
Acute Pancreatitis:
- Serum amylase activity: >130 IU/L suggests acute pancreatitis.
- In acute pancreatitis, the pattern of increase in AMS is as follows:
- Serum Amylase rises within: 2-12 hrs
- Its value peaks at: 24 hrs
- Returns to normal within: 3-5 days
Other causes of hyperamylasemia:
- Inflammation of parotid glands (Parotitis or mumps) results into raised levels of amylase in blood or serum
Serum Lipase (LPS) Activity
Normal: <40 IU/L
Function: LPS hydrolyzes TG to form Fatty acids and Glycerol.
Tissue sources of Lipase:
Rich source of lipase is pancreas.
- Lipase is also released by Ebner's gland and Gastric gland. levels
Therefore, blood or plasma or serum of lipase may be from all of these glands.
Diagnostic significances of Lipase
It is measured in plasma for the diagnosis of acute pancreatitis. Its level rises in pancreatitis similar to amylase.
Acute pancreatitis:
- Serum LPS activity: 2-50 times of URL (upper reference limit) suggests Acute pancreatitis.
- In Acute Pancreatitis, the pattern of increase in LPS is as follows:
- It increases within 4-8 hrs of the onset of symptoms (severe abdominal pain)
- Its value peaks at 24 hrs
- It comes to normal within 8-14 days
- Lipase measurement is done particularly in detecting alcoholic pancreatitis.
Diagnosis of Acute Pancreatitis:
Acute pancreatitis (AP) is one of the most common diseases of the gastrointestinal tract leading to human burden.
For the diagnosis of acute pancreatitis, any two of the three criteria must be present, which are listed below:
- Severe abdominal pain
- Amylase or lipase levels that are three times higher than the upper limit of normal
- Characteristic findings from abdominal Imaging.
Other Tests to detect Pancreatitis
Trypsinogen
Abnormal Results of Trypsinogen in Plasma
Increased levels seen in
- Acute pancreatitis
- Pancreatic cancer
Low levels may be seen in
- Chronic pancreatitis
Fecal Tests:
- Maldigestion and malabsorption occurs if >90% of the pancreas has been destroyed (but early disease diagnosis is not possible).
- Due to deficiency or defect in pancreatic lipase, lipid cannot be digested properly, which in turn leads to impaired absorption of lipid resulting into excretion of fat in feces which is known as steatorrhea.
Radiological studies:
USG (ultrasonography) and CT (computed tomography) scanning can be done for visualization of damage to pancreas.
Cardiac Function Tests
Tests that together indicate a heart's functional capability are called cardiac function tests or cardiac profiles.
Cardiac indicators are a collection of such tests that assess heart function or aid in the diagnosis of heart disease.
Estimating cardiac markers in patient plasma aids in cardiac disease prediction or early diagnosis.
Indications for cardiac function tests
- Ischemic heart disease
- Angina pectoris
- Hyperlipidemia
- Diabetes mellitus
- Hypertension
- Obesity etc.
_1668159672.jpg)
Enzyme Cardiac Makers
- Creatine Kinase (CK) or creatinine phosphokinase (CPK):
- Tissue sources- CK or CPK is present in the cells of skeletal muscle, heart muscle and brain tissues.
- Normal range in plasma: Males: 15-100 U/L and Females: 10-80 U/L
- Diagnostic significance: CK is a sensitive indicator of
- Acute myocardial infarction (AMI)
- Muscular dystrophy and
- CNS disorders
Isoenzymes of CK
CK has three different forms such as CK1, CK2 and CK3 which are present in different tissues but have similar functions.
These three different forms of CK are known as isoenzymes
- CK1 or CK-BB (brain type): It is undetectable (<1% of total CK) in the plasma of normal individuals.
- CK2 or CK-MB (hybrid type): It is present in trace amount (< 6 \% of total CK) in the plasma of normal individuals.
- CK3 or CK-MM (muscle type): It is abundantly present (94-100% of the total CK) in the plasma of normal individuals.
CK-MB:
- It is one of the isoenzymes of Creatine Kinase (CK)
Tissue sources
Significant quantities of CK-MB are present in the cells of myocardium (heart).
Diagnostic significances of CK-MB
- Normal cardiac cell turnover or damage to the cardiac cell results into release of CK-MB in plasma. It means, the more the cell destruction, the more the release of CK-MB in plasma.
- Hence, highly increased levels of CK-MB into plasma is the most specific marker for myocardial damage.
-
CK-MB 26% of total CK: is an indicator of myocardial damage or MI.
-
The pattern of rise of CK-MB after the onset of chest pain or during MI is given below:
Rise within: 4-6 hrs
Peaks at: 12-24 hrs
Returns to normal within: 2-3 day
Aspartate Aminotransferase (AST)
Tissue sources
Cells of cardiac tissue, liver, skeletal muscles.
Diagnostic significances of AST
AST helps in the diagnosis of hepatocellular diseases, skeletal muscle diseases, AMI etc.
Although, AST is not specific to cardiac tissues and is not considered a better marker for cardiac disease, it is included as a cardiac marker because of its property of rising early in plasma after the onset of chest pain.
In AMI:
- AST increases within: 6-8 hrs of onset of chest pain
- Peaks at: 24 hrs
- Comes to normal within: 5 days
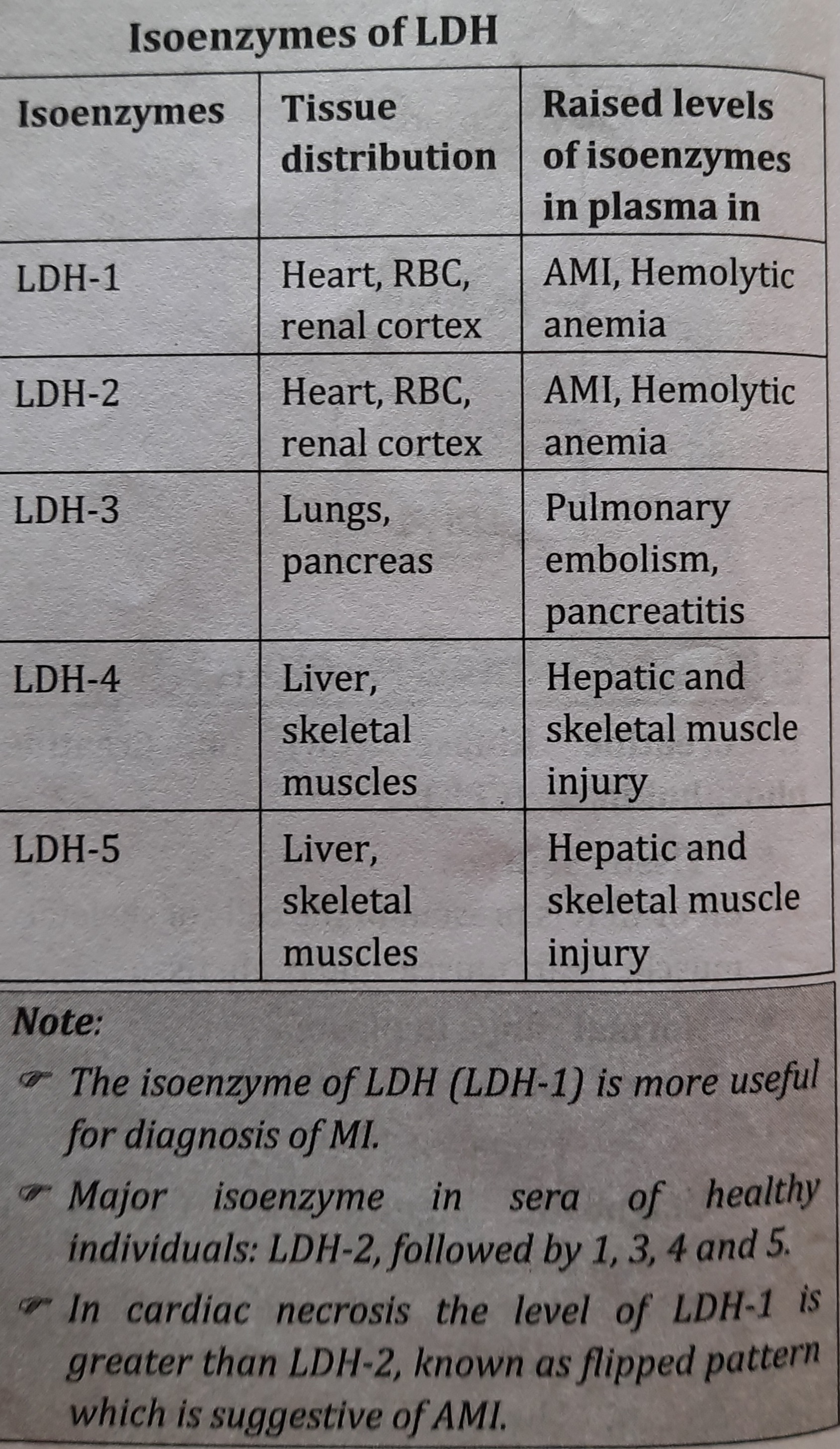
Lactate Dehydrogenase (LDH)
Tissue Sources
High levels of LDH are seen in the cells of heart, skeletal muscle, kidneys, RBCs etc.
- LDH has five isoenzymes, each of which has role in disease diagnosis.
Diagnostic significances of LDH
- Increased activities of LDH are seen in cardiac, skeletal muscle and renal disease as well as in severe hematological and neoplastic disorders.
- LDH helps in the diagnosis MI.
-
The pattern of LDH in MI after the onset of chest pain is as follows:
Rises within: 12-24 hrs
Peaks at: 48-72 hrs
Returns to normal within: 10 days
Things to remember
© 2021 Saralmind. All Rights Reserved.

 Login with google
Login with google