Disinfection of Articles
Subject: Fundamentals of Nursing

Overview
Disinfection of Articles
- Gloves
- Make sure there are no gaps. Use soap and water to clean both surfaces. After that, dry the gloves and dust them with dry powder. After that, it is wrapped in linen, marked separately for the right and left hands, and autoclaved.
- Syringes
- Wash the barrel and piston separately in running water and soap before wrapping each in linen. Put them in an autoclave for 10 minutes at 115°C and 10 lbs of pressure.
- Needles
- The needle should be sterilized with clean water, examined for patency, wrapped in linen with the syringe, and autoclaved. Additionally, it can be sterilized in hot water.
- Bedpans and Urine Pots
- Empty, brush clean, and soak in carbolic lotion (1:40) for two hours, or place in the sun for four to six hours.
- Glass, Stainless Steel, Plastic and Rubber Supplier
- Prior to washing in a hot, soapy solution and boiling or autoclaving, rinse in cold water.
- Sputum Mugs
- Sputum should be collected in a sputum cup with disinfectant lotion. when fully contained. Either boil it or bury it.
- Linen
- After 4 hours, rinse, dry, and send the linen to the laundromat. Keep the linen in a carbolic solution or any other efficient disinfectant.
- Blankets
- The best method is autoclaving.
- Mattresses and Pillow
- Place for two days in the sun's direct rays for six hours each day.
- Mackintosh
- Lysol or Phenol soak for 1:40 or 4 hours, then wash with soapy water and thoroughly rinse. Dry hands in the shade.
- Furniture
- Place in direct sunlight after washing with soap solution or use carbolic to clean.
- Floors and Walls
- Clean the walls you can reach, the windows, the cabinets, and the floors every day with Lysol (1:10) or carbolic
- Thermometers
- After washing with soap, soak for 20 minutes in Savlon 3%.
Central Sterile Supply Department
The CSSD serves as the hospital's central nervous system and is responsible for the decontamination, assembly, sterilization, distribution, and control of all sterile supplies and equipment used throughout the facility.
Objectives of CSSD
- To give various hospital departments with a reliable, affordable, high-quality supply of sterilized supplies in order to provide high-quality, infection-free patient care.
- To successfully complete the sterilizing process.
- To instruct personnel.
- To aid in lowering the hospital infection rate.
- To keep a precise record.
- To keep quality control standards in place.
Structure of CSSD
- There ought to be apart from the normal traffic corridor
- 1 sq. m. per bed
- Zoning: Physical barriers and unidirectional flow should be used. The Central Unit is divided into various zones by two different barriers. On the opposite end, there is a supply window and a collection window.
- In or close to all decontamination, preparation, sterilization, and sterile storage areas, there should be sufficient hand washing facilities.
- In CSSD's sterile zones, there is no exposed overhead piping.
- Avoid being close to drains and sewage pipes when in a sterile area.
- Water supplies should be pure and of high quality. Testing for water hardness should be done every week.
Ventilation requirements
- In the sterile store and processing areas, fans must be installed.
- The ideal HVAC system should be offered to satisfy the following criteria:
- Air flowing in a single direction, from clean to dirty.
- Temperature: +5°C to +18°C
Preparation and Use of Cheatle Forceps
For 20 minutes, immerse the forceps in a 0.5% chlorine solution by boiling (if small) or filling the container. Before using, thoroughly rinse with boiled water, then air dry or sterilize with steam pressure.
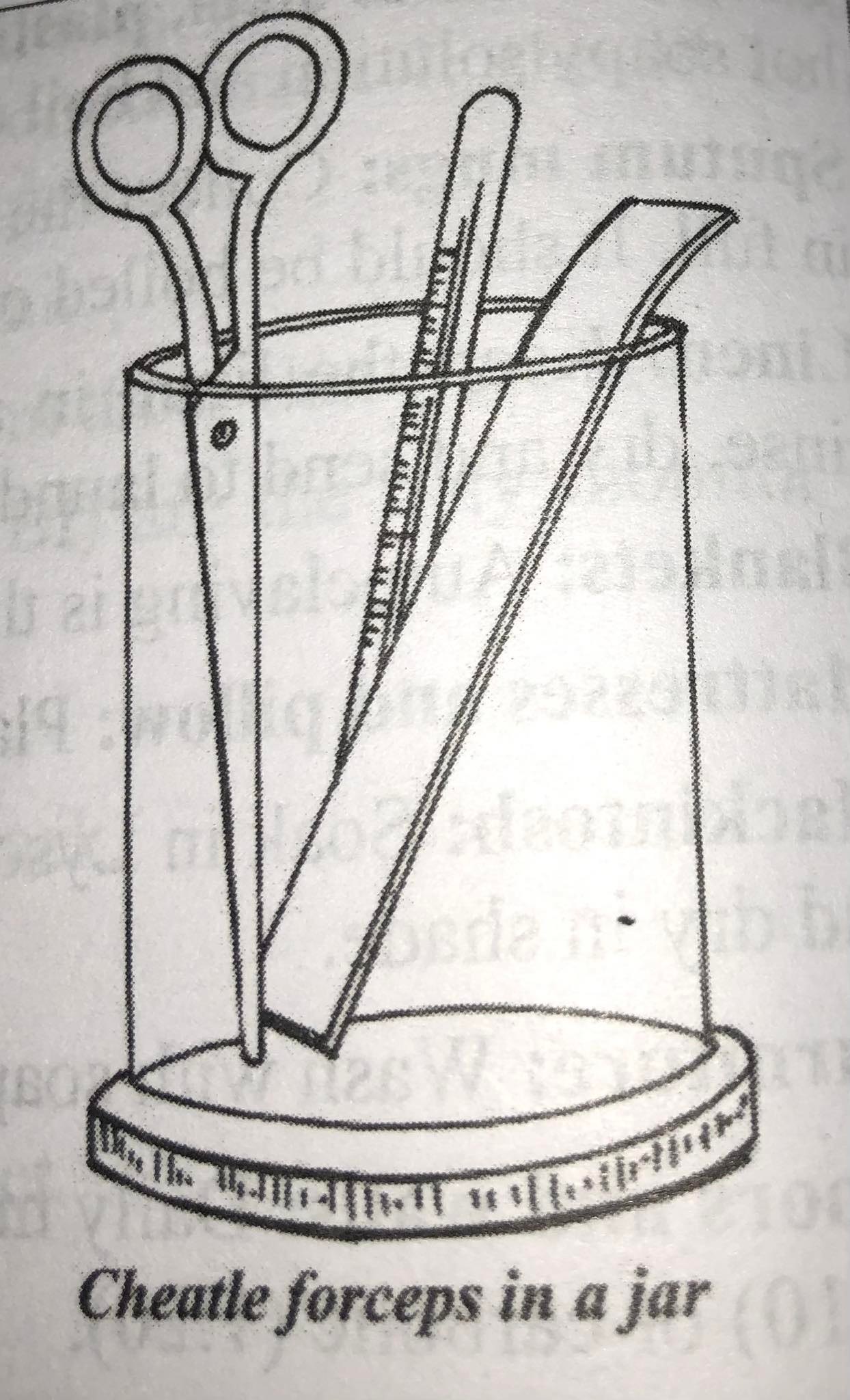
A few recommendations for using cheater forceps
- One jar or container should only hold one pair of sterile forceps.
- Avoid touching the sides of the jar or any other non-sterile surface when removing the transfer forceps from the jar.
- Keep the tip of a sterile forceps horizontal to the handle or below it when using or holding one. Hold it no higher than horizontal.
- To remove extra disinfectant, do not tap the prongs against the container's edge or sides because this could contaminate the prongs.
- To prevent contamination of the inner surface of the lid while removing the sterile objects from the container containing the sterile objects, lift the lid and hold it down; after removing the sterile objects, replace the lid.
- Never put used items back in the container.
- Every day, the jar and forceps need to be sterilized.
- Never move the forceps across the room by yourself.
- Never use non-sterile forceps with sterile equipment.
Hospital Waste Management
"Generation, prevention, characterisation, monitoring, treatment, handling, reuse, and residual disposition of solid wastes" are all parts of waste management. Hospital hygiene and maintenance tasks include waste management. The process is typically carried out to lessen the impact of the materials on health, the environment, or aesthetics. The word typically refers to materials produced by human activity. In addition to municipal (residential, institutional, commercial), agricultural, and special wastes, there are other categories of solid waste (health care, household hazardous wastes, sewage sludge).
Hospital Waste
All garbage produced, wasted, and not intended for further use in a hospital is referred to as hospital waste. Negligent or incorrect handling of medical waste could have detrimental effects on public health. Biomedical waste is defined as "any waste that is generated during the diagnosis, treatment, or immunization of human beings or animals or in research activities pertaining thereto or in the production or testing of biological and includes the waste categories mentioned in the classification of medical waste" in the Bio-Medical Waste Rules, 1998 of India. Medical waste, according to the World Health Organization, is "waste generated by health care activities that includes a broad range of materials, from used needles and syringes to soiled dressings, body parts, diagnostic samples, blood, chemicals, pharmaceuticals, medical devices, and radioactive materials."There are no risks associated with any of the waste products created during medical procedures. Most trash is non-infectious, with between 75 and 90 percent coming from administrative and housekeeping tasks. 10% to 25% of the total hospital waste is designated as harmful and infectious in hospitals. 100% of garbage becomes hazardous when it is combined with nonhazardous trash and not separated at the point of generation. Hospitals, health posts, emergency medical services, healthcare facilities and dispensaries, obstetric and maternity clinics, outpatient clinics, and similar facilities are some of the main sources. Dental offices, psychiatric facilities, salons offering cosmetic piercings and tattoos, and drug addicts are further sources. The waste generated during health-related activities carries a higher risk of injury, infection, and harm than other waste, so it must be properly categorized, segregated, and disposed of.
In Nepal, the majority of hospitals either burn their garbage or simply throw it away. Just throwing it in the municipal garbage stream and burning it can expose people and workers to carcinogens including dioxins and furans. Needlestick injuries brought on by contaminated needles that end up in the trash are one of the main causes for concern. According to a 2000 WHO estimate, contaminated syringes and injections resulted in 21 million cases of hepatitis B virus (HBV), 2 million cases of hepatitis C virus (HCV), and at least 260,000 cases of HIV infection.
Purpose of Hospital Waste Management
- In order to stop the production of garbage.
- To stop sharps injuries from spreading infection to all types of hospital staff and waste handlers.
- In an effort to stop nosocomial infection.
- To avoid spreading illness.
- Drugs are given to anyone handling garbage at any level in order to reduce the danger connected with hazardous chemicals.
- To reduce the danger of waste-related air, water, and soil contamination as well as faulty incineration emissions and ash
- To lessen waste
- To persuade customers not to use disposable products.
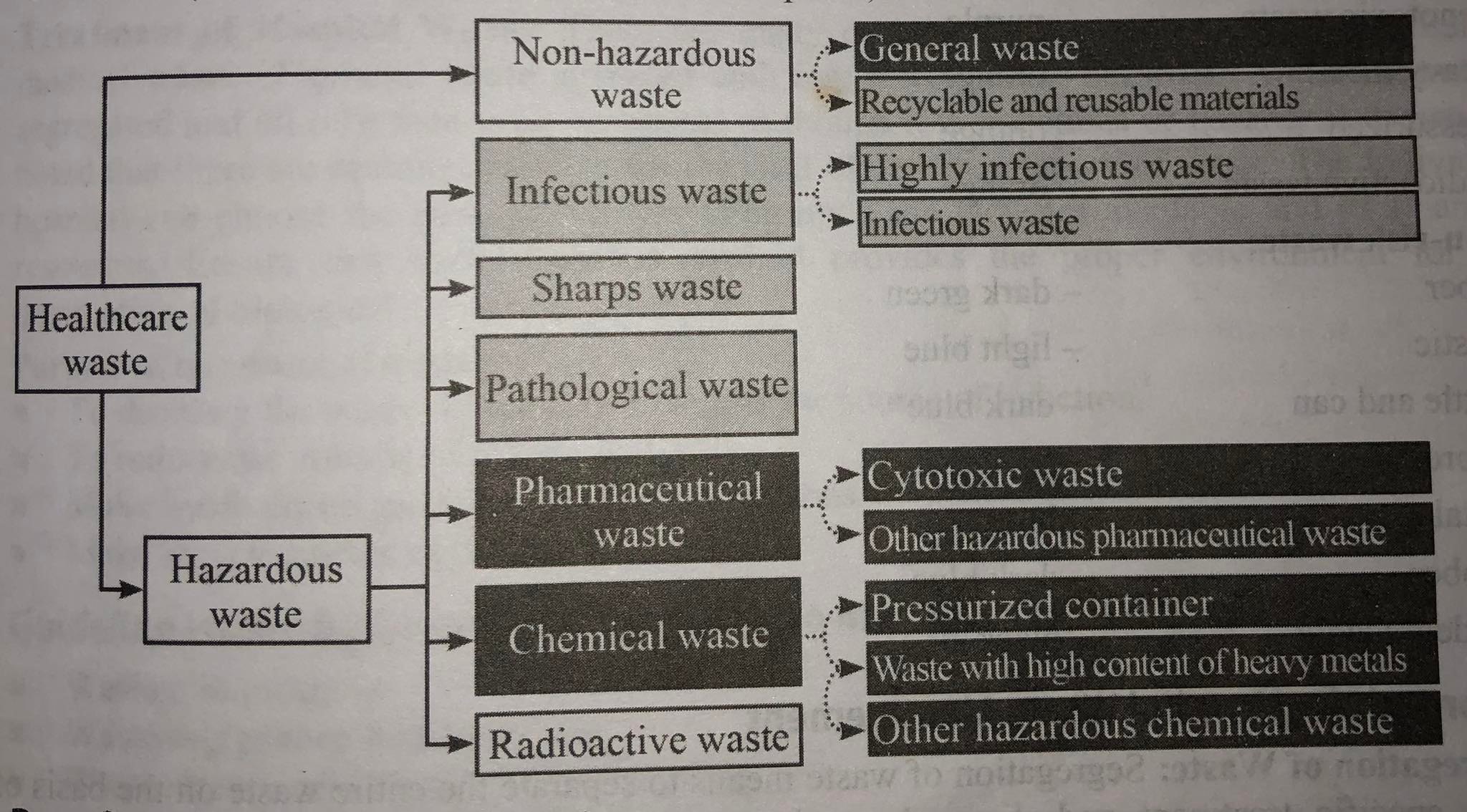
Types of Medical Waste
Both hazardous "healthcare risk waste" and non-hazardous "generic trash" can be used to classify healthcare waste. This contains things like papers, packaging, dust, and similar things. If it has not come into contact with hazardous wastes, it can be disposed of in the same manner as other non-hazardous waste. Sharps (needles, lancets, etc.), syringes, blood or other bodily fluids, contaminated surgical tools, delivery bowls, spent gauze and gloves, plasters, and other potentially hazardous materials make up the remaining 10 to 25 percent of trash. Expired medications, laboratory reagents, and other substances might also be present. Various categories can be used to classify medical waste:
- General Waste
- The majority of it was household or domestic waste. For example, kitchen waste, packaging materials, paper, wrappers, and plastics are all non-hazardous to humans.
- Infectious Waste
- It refers to solid wastes that, when poorly handled, stored, transported, disposed of, or otherwise managed, could fairly be suspected of harboring human pathogenic organisms, pose a significant threat or potential harm to human health or the environment. The majority of medical wastes are sharp wastes. Body fluids and blood come in second. The following list represents the infectious and hazardous solid waste types:
- Biological Wastes
- Blood and blood products, excretions, exudates, secretions, suctioning, and other body fluids, including liquid wastes from renal dialysis, are all considered biological liquid wastes.
- All human tissues and anatomical fragments, including those from human fetal remains, that are produced during surgery, obstetrical procedures, autopsies, and laboratory tests are referred to as pathological wastes.
- Etiologic agent specimen cultures and stocks, as well as related biological wastes from the creation of biological and serums, are included in the definition of "culture and stocks of etiologic agents and connected biological wastes."
- Laboratory waste is defined as waste that has been exposed to pathogenic organisms, blood, or other bodily fluids. Disposable items, culture dishes, transfer, inoculation, and mixing devices, paper and cloth that has come into contact with specimens or cultures that have not been sterilized or rendered noninfectious, or laboratory wastes, such as cultures of etiologic agents, which pose a serious risk to health due to their quantity and virulence, are examples of such wastes.
- Animal tissue, bedding, and other wastes from animals that are known to be infected with a pathogen that also causes disease in humans or that are suspected of being infected with such a pathogen, provided that the available evidence suggests that such tissue, bedding, or waste could serve as a means of transmission to humans.
- Blood lines and dialysate membranes are examples of human dialysis waste.
- Biological waste includes vaccinations and serums made for human or veterinary use by pharmaceutical businesses. These goods may be thrown away due to a bad manufacturing lot (i.e., material that is not up to specification, does not pass quality control, or is recalled), out-of-dateness, removal from the market, or other factors. The discarded material is infectious waste because etiologic agents could be present in these products.
- Sharp Instruments
- It refers to anything thrown away that could cut or pierce someone. Needles, IV tubing with needles attached, scalpel blades, glass slides, glassware, and syringes that have been taken out of their sterile packaging are some examples of these wastes.
- Pharmaceutical Waste
- This includes pharmaceuticals, medications, and chemicals that have been spilled, are no longer in use, or are contaminated.
- Chemical Waste
- This includes discarded cleaning, household, and disinfectant products in the form of solid, liquid, and gaseous chemicals.
- Genotoxic Waste
- Waste containing elements that are genotoxic, such as waste containing cytostatic drugs, which are frequently used to treat cancer, and genotoxic substances.
- Radioactive Waste
- It includes solid, liquid, and gaseous waste contaminated with radionucleides produced by in-vitro examination of bodily fluids and tissues, in-vivo examination of bodily organs, and diagnostic and therapeutic methods for the localisation of tumors.
- Other Infectious Wastes
- It refers to any contaminating soil, water, or other debris left over after cleaning up an infectious waste spill.
- Biological Wastes
- It refers to solid wastes that, when poorly handled, stored, transported, disposed of, or otherwise managed, could fairly be suspected of harboring human pathogenic organisms, pose a significant threat or potential harm to human health or the environment. The majority of medical wastes are sharp wastes. Body fluids and blood come in second. The following list represents the infectious and hazardous solid waste types:
Medical waste can be categorized by the World Health Organization into:
- Sharps
- Infectious
- Pathological
- Radioactive
- Pharmaceuticals
- Others (often sanitary waste produced at hospitals)
Benefits of Waste Management
Waste should not be thrown away or disposed of without thought for its potential re-use. If handled properly through policy and practice, it can be a useful resource. There is a chance to gain a variety of advantages with logical and consistent waste management practices. These advantages consist of:
- Economic
- Enhancing economic efficiency through resource use, treatment, and disposal as well as by developing markets for recycled materials can result in more effective production and consumption practices, the recovery of valuable materials for reuse, and the potential for new employment and business opportunities.
- Social
- By minimizing negative effects on health through proper waste management procedures, the outcomes are more desirable settlements. Better social benefits may result in new employment opportunities and even help communities escape poverty, especially in some of the developing world's poorer cities and nations.
- Environmental
- Improving the quality of the air and water as well as lowering greenhouse gas emissions can be achieved by minimizing resource extraction and reducing or eliminating negative environmental effects.
- Inter-Generational Equity
- Adopting efficient waste management procedures can give future generations a stronger economy, a more equitable and inclusive society, and a cleaner environment.
Containers are colored according to the types of hospital wastes.
According to WHO
- Risk Wastes
- Waste from Infections: Red
- Hazardous waste, pale yellow
- Sharps: Deep maroon/red
- Purple pharmaceutical waste
- Purple genotoxic waste
- Orange heavy metal
- Compressed orange
- Orange radioactive waste
- Non-Risk Waste
- Green-dark paper
- Plastic in pale blue
- Dark blue cans and bottles
- Clear, light-green glass
- Brown metal
- Blue-dark rubber
- Black biodegradable
Approach for Hospital Waste Management
- Segregation of Waste
- To separate all of the waste according to its unique needs for treatment and disposal is to segregate it. At the point where bio-medical waste is generated, segregation should be done because it is the essence of waste management. Only a segregation system can guarantee that trash will be handled in accordance with its level of hazard. Finding the proper disposal route and transportation method for garbage disposal is also helpful. Segregation should be the responsibility of the person who produces the biomedical waste, i.e.docs, nurses, techs, etc (medical and paramedical personnel). The categories listed in the regulations should be used to separate the biological waste. Segregation also includes the practice of separating wastes into different bins according to their color-coding. Separate containers should be placed in distinct hospital wards, such as the medical, surgical, OT, ICU, post-op, etc.
- Collection of Bio-Medical Waste
- Waste management includes the process of waste collecting. The Bio-Medical Waste (Management and Handling) Rules should be followed when collecting bio-medical waste. The collected waste should not be kept for longer than 24 hours at normal room temperature. In order to prevent harm to others, a specific area with a suitable temperature and a distance from people is chosen for its collection.
- Transportation
- To prevent the transit of garbage through the patient care area in the hospital, waste routes must be identified. To lessen the likelihood that biomedical trash would mix with regular waste, separate time should be set out for its transportation. Transporting the garbage to the location for storage or treatment should be done using desiccated wheeled containers, trolleys, or carts. In the event of a spill, or carts should be carefully cleaned and disinfected. The waste should be able to be conveniently loaded and kept secure in the wheeled bins. When being transported, trolleys have no sharp edges and are simple to clean and sanitize. Biohazardous waste that must be transported over a long distance must be kept in containers and properly labeled. Transport is carried out using specially designed desiccated vehicles with fully enclosed bodies that are lined internally with stainless steel or aluminum to provide a smooth, impervious surface that can be cleaned. A bulkhead should be used to divide the driver's compartment from the cargo area. Roof vents should be installed in the load compartment I for ventilation.
Treatment of Hospital Waste
- Medical waste can be treated and disposed of in a variety of ways. When contagious or hazardous garbage is combined with regular waste, it is impossible to separate the two, so everything must be handled carefully. It should be mentioned that there are choices accessible for getting rid of particular waste categories. Depending on the facilities available and its financial capabilities, each hospital can select the best alternative. Make sure that each treatment technique offers the right conditions for the eradication of biological.
Purpose of Treatment of Waste
- To clean the waste so that it can no longer be the infection source.
- To lessen the amount of garbage.
- Make trash invisible for aesthetic purposes.
- Repurpose recycled materials.
Guidelines for Managing Hospital Waste from the Government of Nepal
- Waste reduction
- Waste collection and segregation
- Storage, management, and transportation of waste
- Treatment and disposal of waste
- Providing healthcare professionals with waste management training
Medical Waste Treatment and Disposal Methods
- General Waste
- This group encompasses 85% of the hospital's trash production. The local authority is in charge of properly disposing of this material.
- Bio-Medical Waste
- 15 percent of hospital waste
- Autoclaving
- To sanitize medical equipment, autoclaves are closed chambers that apply heat, pressure, and occasionally steam over time. The Biomedical Waste (management and handling) Rules 1998 additionally mention autoclave and microwave treatment standards for autoclaving and microwave cooking. Sharps and some other infectious waste kinds are often thermally treated in waste management. Waste materials that are contaminated with blood and bodily fluids include cotton, dressings, soiled plaster casts, tubing, catheters, IV sets, and biological toxins, as well as microbiological and biotechnological waste from laboratories, cell cultures, plates, and devices before disposal, autoclave treatment is required. The volume of the processed waste is greatly reduced during the compaction process. The treated garbage can be blended with regular rubbish and disposed of in the usual ways after treatment and compaction. To treat enormous amounts of medical waste simultaneously, massive autoclaves are required. Test kits with a microbiological spore test indication are frequently used to gauge how well the treatments work. Since biological spores are the hardest to kill, the waste is said to have been properly treated when the test package can no longer be cultivated.
- Deep Burial
- Human anatomical waste, such as human tissues, organs, body parts, placentas, etc., is buried deeply in towns with fewer than 5 lakh inhabitants.
- Shredding
- Only after chemical treatment, microwaving, or autoclaving should the plastic (IV bottles, IV sets, syringes, catheters, etc.) and sharps (needles, blades, glass, etc.) be shredded. Needles can be destroyed without any chemical processing by using needle destroyers.
- Chemical Treatment
- Chemical treatment is frequently used to deactivate liquid waste and is intended to disinfect or deactivate specific wastes on-site as opposed to packaging and transporting them to a different facility. It is usually preferable to handle liquids as close to the source of creation as feasible because of how easily they can spill. For handling liquid waste including blood, urine, and sewage from hospitals, chemical disinfection is crucial. Chemicals like chlorine, sodium hydroxide, or calcium oxide can be utilized, depending on the type of waste.
- Microwave Treatment
- Similar to an autoclave, a microwave treatment system similarly uses heat to sterilize medical waste. The moisture in the waste helps the heat to penetrate deeper and the steam sterilizes, making these systems most effective for waste that is not completely dry or solid.
- Incineration
- By converting organic and combustible trash to inorganic incombustible matter using a high-temperature, dry oxidation process, waste volume and weight are significantly reduced. Pharmaceutical and pathological waste are routinely burned, and the state frequently mandates this practice. When treating waste that cannot be recycled, reused, or disposed, this procedure is typically chosen. To achieve full combustion and reduce any unfavorable environmental consequences, medical waste should be incinerated in a controlled setting.
- Land Disposal
- Most shredded, processed, and decontaminated garbage is disposed of on land. When other methods of decontamination are ineffective, it may also be employed for hazardous waste or other untreated waste. Specialized sanitary landfill sites offer a secure environment for the disposal of medical waste while lowering the danger of soil and water contamination.
- Inertization
- In order to reduce the risk of toxic waste contained in the waste, the intertization process involves mixing waste with cement and other substances before disposal, such as 65% pharmaceutical waste, 15% lime, 15% cement, and 5% water.
Measures for Waste Minimization
Purchase of reusable items made of metal and glass should be promoted as much as is practical. The "3 R's" - reduction, reuse, and recycling - are practices that help reduce waste.
- Minimizing the quantity of waste produced by a certain operation or process is referred to as reduction. It is achieved by switching out highly polluting products for less polluting ones, by employing procedures that produce less waste, and by following best practices. In reality, source reduction is more about managing the raw materials more carefully in the first place than it is about controlling waste.
- Reusing something means using it exactly as it is, like utilizing waste oil as fuel.
- Recycling is the process of recovering materials from waste items, such as recycling scrap metal or creating new products out of waste plastic or paper. The advantages of recycling are numerous. It conserves natural resources, lessens the amount of waste that needs to be disposed of, and gives scrap traders and collectors work.
General Guidelines and Safety Measures
- Other wastes shouldn't be combined with biomedical waste.
- Prior to being stored, transported, treated, and disposed of, it should be divided into containers at the place of generation.
- When performing therapeutic and diagnostic procedures as well as when handling biomedical waste, all producers of biomedical waste should follow general safety precautions.
- Contaminated waste must be collected and transported in leak-proof containers to disposal locations.
- To inform handlers of segregation at the source, use color coding.
- The nature and risk of the trash should be known to the drivers, collectors, and other handlers.
- Regarding the methods to be used in the event of spills or accidents, written instructions are supplied.
- Protective equipment is offered, and usage instructions are provided.
- Waste should be moved when there are the fewest visitors, which is early in the morning or late at night.
- Biomedical waste that has not been handled must not be retained for longer than 48 hours.
- Tetanus and hepatitis B vaccinations provide workers with protection.
- Every hospital needs to have a well-thought-out awareness and training program for all job categories, including administrators (medical, paramedical and administrative).
- The Bio-medical Waste (management and handling) Rules of 1998 must be made known to all medical personnel.
- To provide prizes for effective universal safety measures and safe hospital waste management.
- All staff types should get training in a suitable setting and in the appropriate language and medium.
- A hospital waste management committee should be established in each hospital, led by the institute's director and including substantial representation from all key departments. This committee should be in charge of developing a hospital-specific action plan and overseeing, monitoring, and implementing it. The annual reports and accident reports that are required by BMW regulations should be submitted to the relevant authorities in accordance with BMW regulations.
Things to remember
© 2021 Saralmind. All Rights Reserved.

 Login with google
Login with google