Infection Control Measures
Subject: Fundamentals of Nursing

Overview
Decontamination and cleaning techniques are used to lower the amount of microorganisms and stop their transmission from one location or person to another. This is what is meant by the term "infection prevention." Due to their poor immunity, the presence of microorganisms in the environment, and invasive procedures used during treatment, patients entering a healthcare setting are at risk of contracting infections. Health professionals must take precautions to safeguard both themselves and their patients and visitors since they operate in an environment where infections are always present. All healthcare professionals should be aware of infection control measures. It is the duty of nurses to deliver high-quality care that includes infection control measures.
Terminology of Infection Prevention
- Aseptic Technique:
- The efforts made to stop the entry of microorganisms into any area of the body where they are likely to cause infection are collectively referred to as aseptic techniques or asepsis in healthcare settings.
- Sepsis:
- A compound form with a meaning related to decay or infection.
- Infection:
- An infection is a clinical illness brought on by the invasion and proliferation of a pathogen in the body. It results from an interaction between an infectious agent (bacteria, viruses, fungi, or parasites) and a vulnerable host. It is when pathogens, such as microorganisms that multiply quickly and cause diseases, infiltrate the body.
- Local Infection:
- It is restricted to the region of the body where the microorganisms are still present.
- Systemic Infection:
- If the microorganism spreads and harms various body parts.
- Host:
- It is a live organism that is housing another organism as a parasite, usually giving that organism food and shelter so it can develop to adulthood and breed. An organism that can be impacted by an agent is a host.
- Agent:
- Diseases are brought on by biological pathogens, such as viruses, parasites, fungi, or bacteria, as well as toxins or toxic chemicals.
- Antisepsis:
- Antisepsis is the use of a chemical agent to kill or inhibit microorganisms on skin and other body tissue in order to prevent infection.
- Antiseptic:
- It is a chemical that tends to prevent the microbe from growing and reproducing.
- Cleaning:
- Cleaning is the process of physically removing any traces of blood, bodily fluids, or other foreign substances from skin or inanimate objects, such as duster dirt.
- Disinfectant:
- It is a chemical that kills pathogenic bacteria, but not necessarily all others, when applied to inanimate items.
- Disinfection:
- Disinfection is the process that gets rid of the majority of disease-causing microorganisms, but not all of them. All microorganisms are removed by high level disinfection (HLD), which can be done chemically or by boiling, with the exception of bacterial endospores.
- Decontamination:
- Before cleaning, decontamination is the process that makes items safer for people, especially cleaning professionals, to handle. Among these items are ones with a wide surface area, such an operating table, as well as gloves used during or after surgery that have been contaminated with blood or bodily fluids.
- Sterilization:
- The procedure that gets rid of all microorganisms, including bacterial endospores, is sterilization.
- Bacteremia:
- Bacteremia is the medical term for the illness where a blood culture of the patient reveals microorganisms.
- Septicemia:
- Septicemia is the term used when bacteremia leads to a systemic infection.
- Acute infection:
- Usually starts off unexpectedly or only lasts a short while.
- Chronic Infection:
- May develop slowly over a very long time and last for several months or a whole year.
- Nosocomial Infection:
- Nosocomial infections are infections that occur as a result of providing medical care inside a hospital or medical facility. Health professionals working in the facility could possibly contract nosocomial infections including hepatitis B, HIV, etc.
- Droplet Infection:
- It is the infection of people through tiny droplets of saliva and mucus that are released during coughing, sneezing, or speaking from another person's mouth and nose.
- Inflammation:
- There are five symptoms that describe this localized, non-specific defensive response of the tissues to injury or infection.
- Bactericidal:
- Bactericidal substances kill microorganisms.
- Bacteriostic:
- It is a substance that stops bacteria from growing but does not actually harm the bacteria.
- Sterilization:
- All microorganisms, including their spores and pathogenic and non-pathogenic varieties, are destroyed during this process.
Chain of Infection
An infection is the result of pathogens or other microbes invading the body. An infectious disease is brought on by the interaction of an agent, a host, and an environment. Most of these diseases develop along a typical infection chain that ends with an infected host. The infection chain, which consists of its six components, is a part of this cycle. Understanding the chain of infection can help with both infectious illness prevention and treatment.
Disease Transmission Cycle
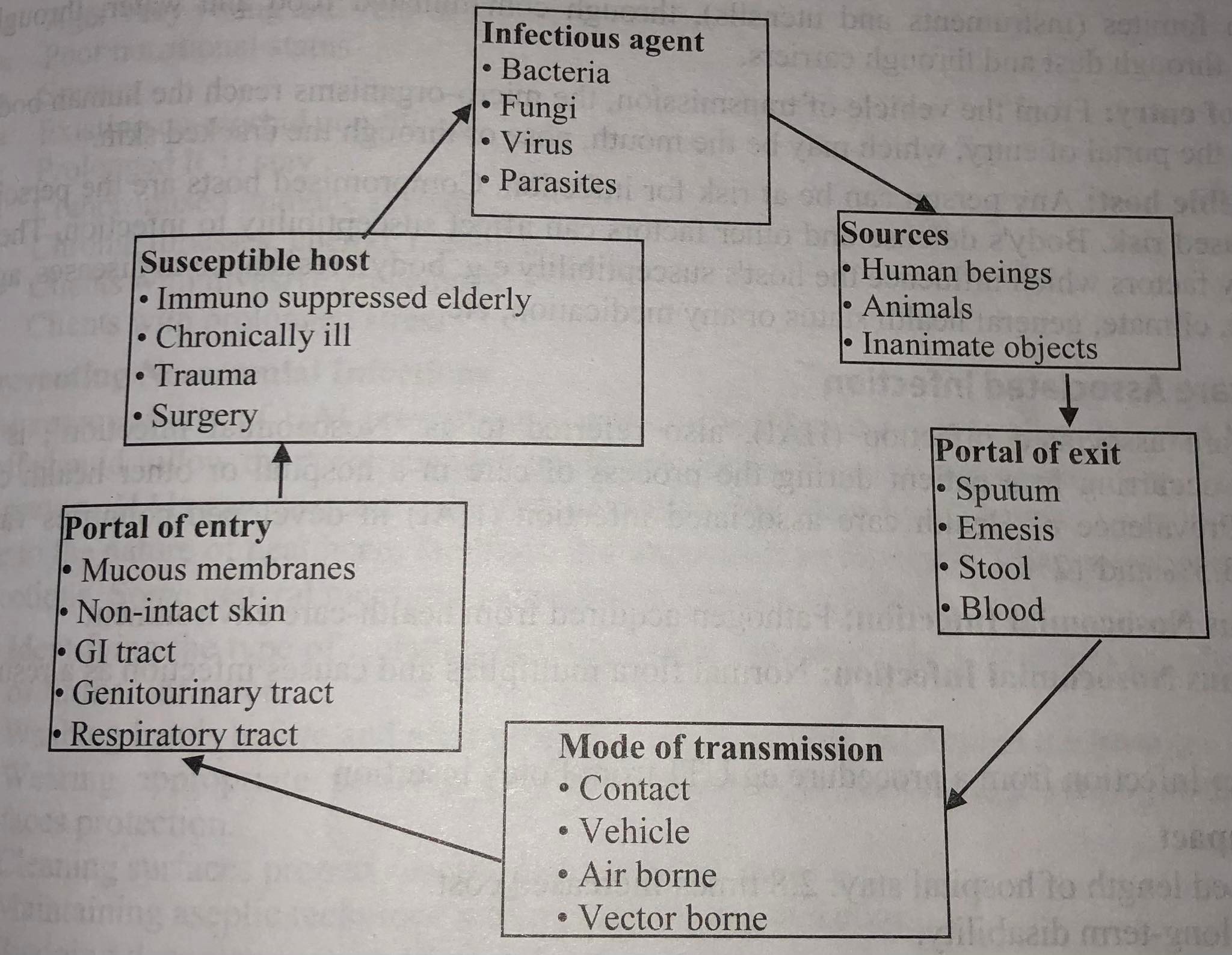
- Infectious Agent:
- An infectious agent that is a microbiological agent, such as a bacterium, virus, fungus, or parasite, is the first link in the chain of infection. Pathogenicity, virulence, invasiveness, and specificity are all factors that influence an infectious agent's capacity to spread disease. Pathogenicity refers to an organism's capacity for harm and disease transmission, whereas virulence refers to the organism's zeal for growth and multiplication. The ability of an organism to invade tissues is referred to as invasiveness, and its attraction to a particular host, which may include people, is referred to as specificity. An infection is more likely to occur when an organism is more pathogenic, virulent, and invasive than the body's natural defenses.
- Reservoir (source):
- A pathogen can persist in a reservoir, where it may or may not reproduce. Sources include inanimate objects, people, and animals. Medication, air, food, water, and any other substance that an organism can feed on or rely on to remain inactive are examples of inanimate items. Other clients, healthcare professionals, family members, guests, and clients themselves are examples of human sources. For instance, humans are the reservoir for tubercle bacilli and syphilis spirochete. The organisms that cause tetanus and gas gangrene are found in soil.
- Portal of Exit from Reservoir:
- The microorganism must depart from the reservoir before an infection can take hold in a host. Common human reservoirs and their corresponding departure points include the mouth, urethra, vagina, wound, and others.
- Mode of Transmission:
- A microorganism needs a mode of transmission once it has left its reservoir source in order to enter another individual or host through a portal of entrance.
- Direct Transmission:
- The organisms can be spread directly from one person to another by sexual contact, diseased hands, droplet infection, and other means.
- Indirect Transmission:
- Coming into contact with the secretions and excretions of the infected individual through fomites (tools and utensils), tainted food and water, insects, dust, and carriers.
- Portal of Entry:
- The microorganisms enter the human body from the vehicle of transmission through the portal of entrance, which can be the mouth, nose, or a skin wound.
- Susceptible Host:
- Anybody is a potential host who is susceptible to infection. The people that are at higher risk are the compromised hosts. Susceptibility to infection can be influenced by the body's defenses and other elements. Numerous factors, such as the host's body's resistance to diseases, age, sex, race, climate, general health state, or any medicine, etc., affect the host's vulnerability.
Healthcare Associated Infection
An infection that develops in a patient while they are receiving treatment in a hospital or other healthcare facility is known as a health care associated infection (HAI), also known as a "nosocomial infection". In wealthy nations, the prevalence of healthcare-associated infections (HAI) ranges from 3.5% to 12%.
- Exogenous Nosocomial Infection:
- Pathogen acquired from health-care environment
- Endogenous Nosocomial Infection:
- Normal flora multiplies and causes infection as a result of treatment
- Latrogenic:
- Infection from a procedure eg UTI from Foley insertion
Health Impacts:
- Extended hospital stay: 2.8 times longer cost increases.
- Long-term disability creation.
- A rise in antimicrobial resistance.
- Represent a significant monetary burden for health systems.
- Primary factor in dying.
Type of Nosocomial Infections:
- Urinary Tract Infections (UTI).
- Surgical Site Infections (SSI).
- Respiratory Tract Infections (RTI).
- Blood Stream Infections (BSI).
- Ventilator Associated Infections (VAP).
- Skin Infections (SI).
- Gastrointestinal Tract Infections (GI).
- Central Nervous System Infections (CNS.
Causes
- Improper medical or Surgical Asepsis.
- Insertion, drainage system contamination, and inadequate cleaning can contribute to urinary tract infections.
- An improper method of hand cleaning or changing a bandage at a surgical site.
- Improper hand washing or suctioning method might cause upper respiratory infections.
- Improper hand cleansing or site maintenance during intravenous.
- A prolonged hospital stay of one day.
- Numerous caregivers.
- Antibiotic usage and selection.
- Incorrect surgical or medical asepsis.
Risk for Nosocomial Infection:
- Age: Very young and very old.
- Poor nutritional status.
- Smoker.
- Existing co-morbid conditions.
- Prolonged ICU stay.
- Compromised immune system.
- Chronic illnesses, chemo, radiation.
- Clients with invasive procedures.
- Clients with prolonged stress.
Preventing Nosocomial Infections
The healthcare establishment bears duty for HAI prevention. Hospitals and medical personnel should adhere to the prescribed standards for cleaning and sanitization. Your risk of developing HAIS can be reduced by 70% or more by taking precautions. It is however hard to completely eradicate nosocomial infections due to the nature of healthcare institutions. Following are a few common infection prevention strategies:
- Determining the appropriate sort of isolation that will protect others or lessen the risk of infection.
- Touching patients in the hospital and washing hands both before and after procedures.
- Wearing the proper personal protective gear, such as gloves, gowns, boots, and face shields.
- Adequate surface cleaning at the recommended intervals.
- Observing aseptic technique when carrying out the process
- By decontaminating the contaminated equipment.
- Ensuring adequate ventilation in the space.
Maintaining of "Protective Barriers".
Placed between the host and the microbes are barriers:
|
Microbes
|
Barriers
|
Host
|
Asepsis
It is the strategy utilized to prevent infectious organisms from coming into touch with the patient's environment. It consists of a sequence of procedures, each of which is completed in a germ-free environment to maintain the sterility of the entire process. Surgical asepsis and medical asepsis are the two aseptic techniques that nurses frequently employ.
Principles of Asepsis:
The aseptic practices and principles must be adhered to by all workers involved in an aseptic procedure. The principles of sterile technique cover all procedures used to preserve sterility as well as control and prevent infection, stop the spread of all germs in a specific region, and control and prevent infection. All healthcare professionals have a duty to speak up and keep all patients free from infection.
- Prior to any aseptic procedure, hand cleanliness must be prioritized.
- When performing a procedure, make sure the patient is aware of how to keep the equipment clean and knows not to make sudden movements, touch, laugh, sneeze, or talk while in the sterile area.
- To reduce the spread of pathogens from patients to healthcare professionals, choose the proper PPE.
- Before beginning any invasive surgery, familiarize yourself with the hospital's policies and regulations for sterile technique.
- If possible, invasive procedures should be avoided by healthcare professionals who are ill; otherwise, they should double mask.
- Prior to use, examine the intactness, dryness, and expiration date of the packaging to ensure sterility.
- Non-sterile packaging includes any that has been torn, washed, opened, dropped to the ground, or is wet.
- Only sterile tools or sterile gloves should ever come in contact with sterile objects.
- The gravity-directed flow of fluid. During sterile procedures, keep forceps' tips down to avoid fluid from covering the entire forceps and potentially contaminating the sterile field. Maintain all sterile tools and gloves above the level of the waist.
- Sterilized trays should be set up as near to the time of usage as possible. By being exposed to airborne germs for an extended period of time, sterile things can become non-sterile.
- A sterile barrier must be regarded as contaminated if it is broken, gets wet, or tears. Maintain a dry sterile surface; replace it if it becomes damp or torn.
- Items that are not sterile should not enter the sterile area. A non-sterile person shouldn't, for instance, reach over a sterile field.
- To prevent contamination, use best practices when opening sterile equipment or adding supplies to a sterile field.
- Do not laugh, sneeze, cough, or talk while in the sterile area.
- Keep sterile and non-sterile items and spaces separated by a safe distance or margin of safety.
- Keep doors locked and limit traffic in the operating room (OR).
Medical Asepsis
The term "medical asepsis," sometimes known as "clean method," describes procedures intended to lessen the amount of pathogenic germs and restrict their growth and transmission in the patient's environment. It is "a level of cleanliness that lessens the likelihood of the transmission of illnesses."
Purposes of Medical Asepsis:
- To aid the patient in battling an existing infection and halt its progress.
- To stop the patient from contracting the same pathogen again.
- To avoid the patient contracting a brand-new pathogen.
- To avoid spreading an infection to visitors and medical personnel who come into contact with the patient.
- To lessen the risk that the patient will develop a nosocomial infection and pass away from one they contracted while in the hospital.
Medical Asepsis Includes
- Clean technique:
- Maintaining a clean environment
- Maintaining clean hands
- Changing a client's linen daily
- Cleaning equipment
- Isolation precaution:
- Transmission based precautions, Barriers technique (e.g. PPE)
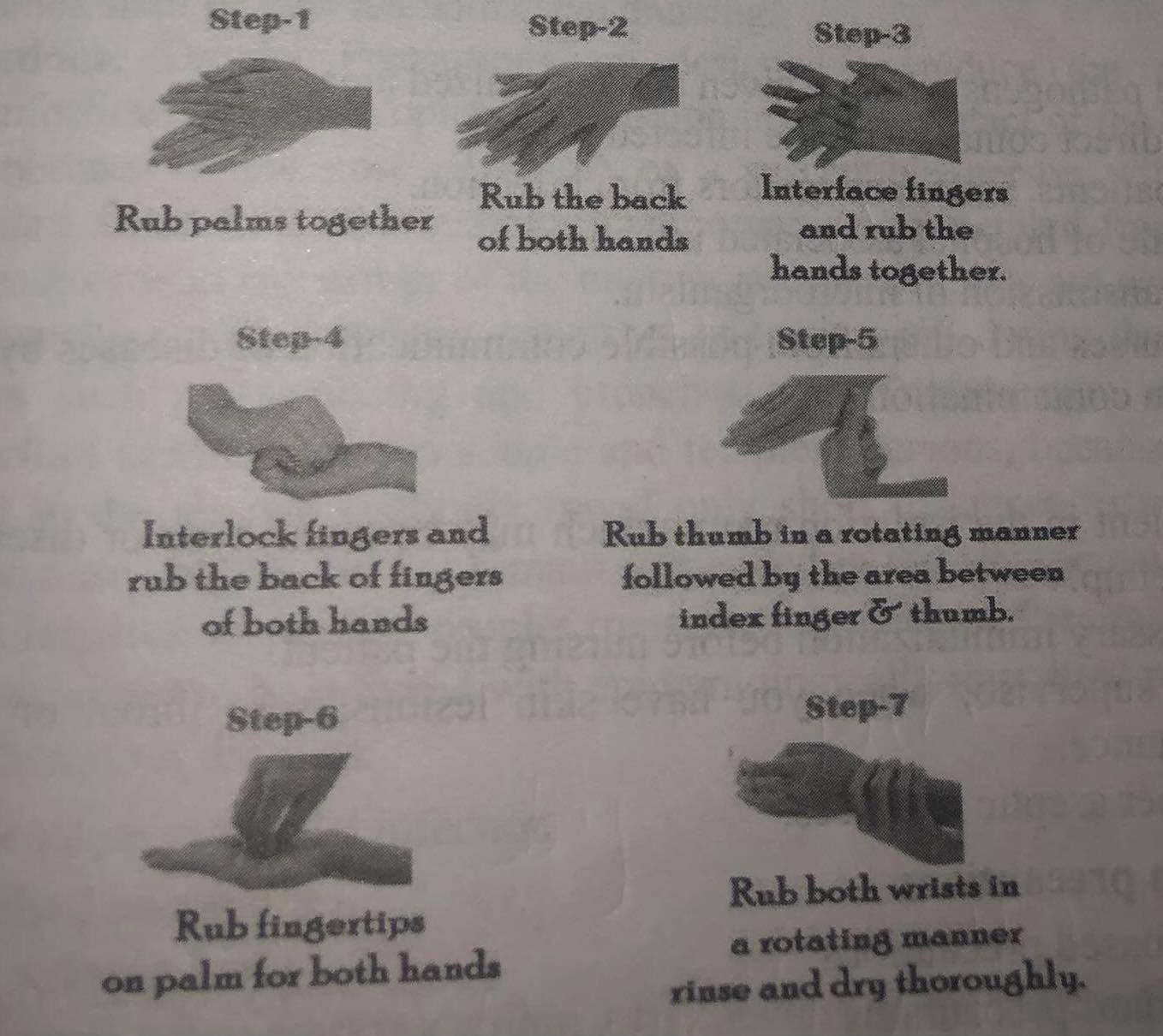
Hand Hygiene
Both mechanical and chemical actions are involved in hand cleaning. Even though practicing good hand hygiene is the most effective preventive measure for reducing hospital acquired illnesses, it is occasionally neglected. By washing our hands and using hand sanitizer (an alcohol-based hand rub that contains 60% to 90% isopropanol, ethanol, or a combination of the two), we can keep our hands clean.
Hand Washing:
Cleaning your hands with the intention of getting rid of dirt, debris, and microbes is known as hand washing. The amount of bacteria is reduced by thorough hand washing. The easiest and most crucial step in preventing hospital acquired infections is washing your hands. Hand washing with soap and running water removes around 80% of germs.
Purposes:
- To clean hands of dirt and stray microorganisms.
- To lessen the possibility of spreading bacteria to patients.
- To lower the possibility of patients getting sick from each other.
- Gatrogenic infections should be avoided.
Articles:
- Soap/antiseptic detergent.
- Running warm water.
- Nail brush in antiseptic lotion.
- Towels (sterile)/drier.
Indications:
The WHO has "five Moments" for washing hands:
- Before patient care.
- After environmental contact.
- After exposure to blood/body fluids.
- Before an aseptic task.
- After patient care.
The following are typical prerequisites for hand washings:
- After arriving at the hospital and finishing shifts of duty, before beginning work.
- Prior to, during, and following all physical interactions with the patients.
- Before beginning any type of procedure, both invasive and noninvasive.
- Prior to administering medication, preparing, or serving meals.
- After touching bandages and linens, or unclean and contaminated equipment (urinals, bedpans).
- Both before and after specimen collection.
- After caring for patients with AIDS, typhoid, hepatitis, or patients who are isolated, as well as after handling objects from such a room.
- After using the restroom.
- Following a nose blow.
- After dealing with trash.
- Even if gloves are worn, after handling circumstances where microbiological contamination is possible.
Guideline for Hand Washing:
- In a non-surgical situation, wash for at least 15 seconds; in a surgical setting, wash for 2–6 minutes.
- When wearing jewelry, it's challenging to properly wash your hands. Jewelry should ideally not be worn in a therapeutic setting.
- Try to use warm water.
- Microorganisms must be eliminated using friction, flowing water, and a cleansing chemical.
- Using soap when washing your hands helps to keep your hands clean by removing dirt and microorganisms.
- Clean between your fingers.
- In order to minimize dirt and microorganisms, nails should be kept short.
- Cuff sleeves up above the elbow (if necessary)
- Remove nails, especially when washing your hands after surgery.
- Once the hands have been thoroughly washed, they are dried with a sterile towel or an air dryer.
- Five times through each of the six hand-washing stages.
Even though hand washing is the most effective preventive measure for reducing hospital acquired illnesses, it is occasionally not done properly. The joint Commission and the Quality and Safety Education for Nurses (QSEN) project, both funded by the Robert Wood Johnson Foundation (RWJF), are working to address the issue of supplying incoming nurses with the information, abilities, and perspectives required to continuously enhance the quality and safety of the healthcare systems in which they will work. Effective hand washing is one method for achieving this objective.
Types of hand washing:
- Medical hand washing:
- Cleaning your hands with soap and water before and after completing any tasks is known as "medical hand washing." It cleans the bacteria off the hand's surface and can stop the spread of diseases.
- Surgical hand washing:
- Surgical hand washing is a technique used to mechanically and chemically remove dirt, bacteria, and other microorganisms from hands and fingers before surgery.
- Alcohol hand washing:
- Alcohol hand washing is a technique for disinfecting hands using an antiseptic solution. If there is no running water and frequent hand washing is required, this method works quite well.
Method of Hand Washing:
Steps:
- Take off all of your rings, bracelets, watches, and other jewelry.
- Set the flow and temperature of the water after turning it on.
- Hands should be fully wet before applying soap or liquid soap.
- Hands are commingled. Rub your right hand's thumb and finger tips in your left hand's palm and vice versa in a circular motion.
- Rub palms together.
- Place the left palm on the right dorsum and the right palm on the left dorsum (rub back of the hand).
- between your fingertips.
- Rub opposing palms together while keeping your fingers interlaced.
- Rub your thumb's base.
- Make circular motions with the fingernail.
- Swipe wrist.
- Rinse hands thoroughly under running water to remove all soap.
- When no clean towel is available, air-dry your hands or use a clean paper or cloth towel to dry your hands. It may be used at both the home level and in healthcare facilities, and it only takes around 30 to 35 seconds.
For surgical hand washing:
- After washing your hands, put on a cap and a mask.
- Knee, foot, or elbow to activate the water.
- Lather soap or detergent to a height of 5 cm above the elbows on your hands and forearms (hands must always be held above the elbows). Wash the palms, backs of hands, wrists, forearms, and interdigital regions for 20 to 25 seconds using firm circular motions.
- Rinse both of your hands and your forearms from the tip of your fingernails all the way down to your elbows.
- Use a nail pick or nail brush to clean between the nails on both hands.
- Use an antibacterial agent to 15 times scrub the nails on each hand.
- With the brush held perpendicular, scrub the palm, 10 times each on the thumb, fingers, and back of the hand.
- Rub the wrist, upper forearm, antecubital fossa, and marginal area above the elbows from wrist to 5 cm above each elbow.
- Five to ten minutes should be allotted for the scrub.
- Throw away the brush and thoroughly rinse your hands, elbows and all.
- During the process, be careful not to touch the sink's sides or the tap.
- Dry one hand, working from the fingertips to the elbow, using a sterile towel. Dry the area from the cleanest to the dirtiest.
- Using a different towel, dry the other hand once more. If there is only one towel available, use one side for your other hand.
- Put on a sterile gown and continue.
Things to remember
© 2021 Saralmind. All Rights Reserved.

 Login with google
Login with google