Pulse
Subject: Fundamentals of Nursing

Overview
Pulse
The wave of artery expansion and contraction brought on by the heart's pumping motion is known as a pulse. The heart rate, or the number of times the heart beats each minute, is gauged by the pulse rate. The arteries enlarge and constrict with the flow of blood as the heart pumps blood through them. Heart muscle is stimulated to contract by electrical impulses that come from the sinoarterial node. Each time the ventricles contract, 60 to 70 ml of blood enter the aorta. The aorta's walls swelled with each stroke volume ejection, generating a pulse wave that swiftly moved toward the distal ends of the arteries.The wave travels through the aorta 15 times quicker than the expelled blood volume does, and through the tiny arteries 100 times faster. We may feel when a pulse wave enters a peripheral artery by softly pressing the artery against underlying bone or muscle. The felt limit of the blood flow in the peripheral artery is the pulse. The pulse rate is the number of times your body pulses in a minute.
Characteristics of Pulse
Pulse Rate: It is the number of pulse beats per minute. The normal pulse rate in adults varies from 72 to 80 beats per minute. 31 5520 els bra
- Pulse rate before birth 140-150/m.
- Pulse rate new born 130-140/m.
- Pulse rate 1st year 115-130/m.
- Pulse rate 2nd year 100-115m.
- Pulse rate 3rd year 90-100/m.
- Pulse rate 4th-8th year 86-90/m.
- Pulse rate 8th-15th year 80-86/m.
- Pulse rate at adult 70-80/m.
- Pulse at old age 60-70/m.
Adults with resting pulse rates of more than 100 beats per minute are said to have tachycardia, which often denotes an unhealthy condition. Bradycardia is defined as a pulse rate of fewer than 60 beats per minute. Take into account the various variables that might affect pulse rate while evaluating the pulse.
Rhythm or Regularity: The amount of time between pulse beats is known as pulse rhythm. The intervals between heartbeats are usually equal or regular. The pulse is referred to as irregular or arrhythmic if the time intervals are not equal or regular. For a full minute, count your pulses to look for any arrhythmias. An irregular rhythm, or dysarrhythmia, is indicated by an interval that is broken by an early or late beat or a missing beat.
Tension: The degree of compressibility is determined by the arterial wall's resistance. An artery is considered to have high tension when it is challenging to compress it, and low tension when it is simple. The arteries often lose their flexibility and harden as a person ages. When taking someone's pulse, such arteries are harder for the fingers to squeeze.
Strength/Volume: It is the fullness of artery. It is force of blood felt at each beat. It can be either full or weak. A normal amount of blood in artery causes the pulse to be full. If the amount of blood in the artery is decreased as in hemorrhage or dehydration, the pulse becomes feeble, thready or weak.
Common Sites for Taking Pulse
Any accessible artery can be assessed for pulse rate but the radial and carot commonly used because they are easily palpated.
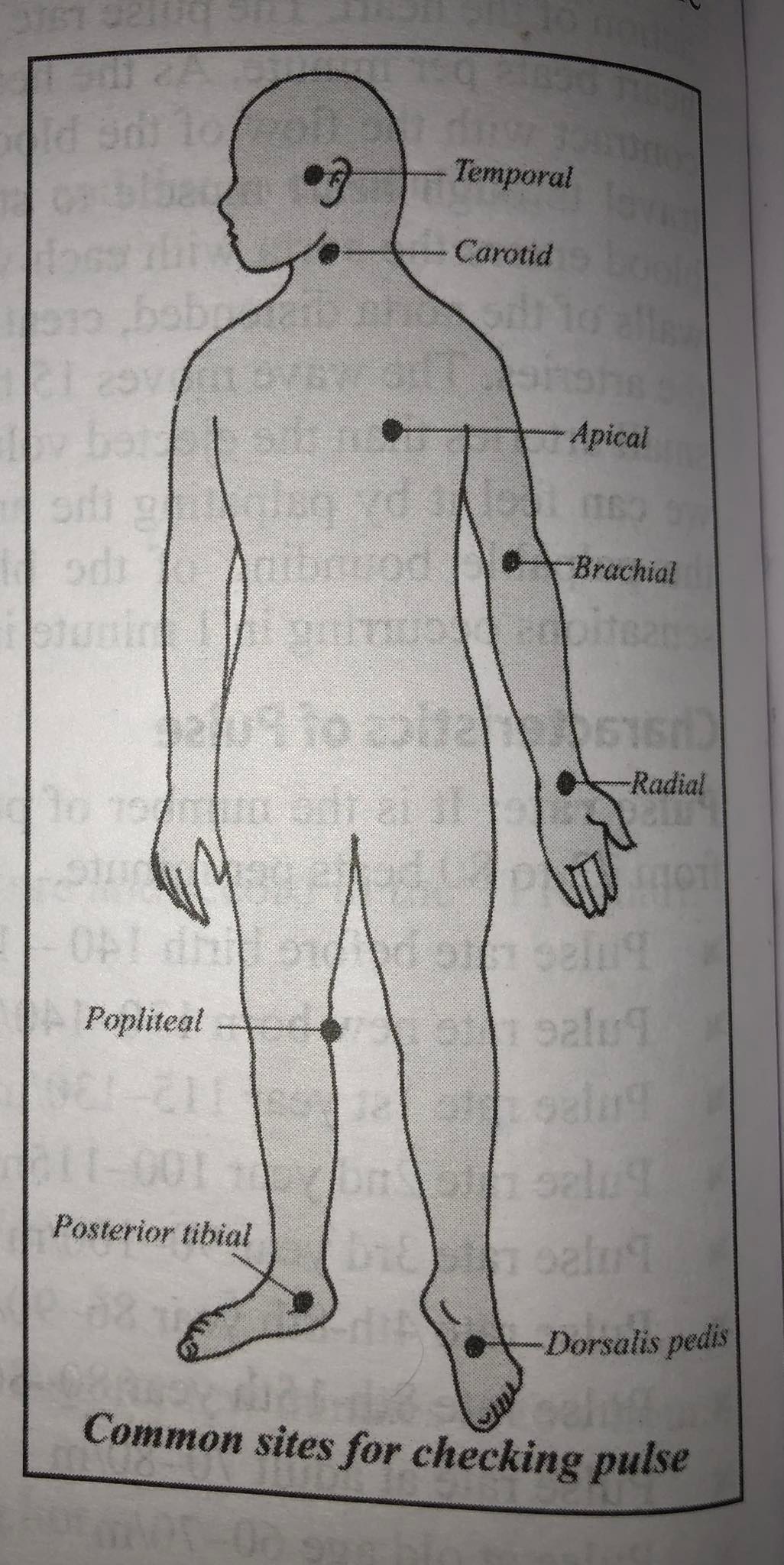
Radial: Inner aspect of the wrist on thumb side. It is common site used to assess character of pulse peripherally and assess status of circulation to hand.
Temporal: Over the temporal bone or superior and lateral to the eye. It is easily accessible site used to assess pulse in children
Carotid: At the side of the trachea along medial edge of sifted 1 sternocleidomastoid muscle in neck. It is easily accessible site used during physiological shock or cardiac arrest.
Apical: Left side of the chest in the 4th, intercostals space in the midclavicular line. 5th or 6th
Ulnar: Ulnar side of forearm at wrist. Site used for assess status of circulation to hand and also used to perform an Allen's test.
Brachial: Medially in the antecubital space, above the elbow.
Femoral: Below inguinal ligament, midway between-001 symphysis pubis and anterosuperior illiae spine. It is used to assess character of pulse during physiological shock or cardiac arrest and to assess status of circulation to leg.
Popliteal: Medial or lateral to the popliteal fossa with knees slightly flexed, used to assess status of circulation to leg.
Tibial: On the medial surface of the ankle behind the medial malleolus, used to assess status of circulation to foot. albar band
Facial: At the outer angle of the lower jaw.
Dorsalis Pedis: Along dorsum of foot between extensor tendons of great and first toe, used to assess status of circulation to foot.
Factors Affecting the Pulse
There are many internal and external factors that can cause heart rate to fluctuate.
Age: A person's pulse rate becomes slower as he gets older. Very old person have slow pulse rate and children will have faster beat.
Sex: Females have a slightly higher pulse rate than males.
Exercise/Activity: It is much faster during exercise. Exercise or any type of physical exertion, is the healthy response as the body and muscles demand increased oxygen levels. Heart conditioned by long term exercise, resulting in lower resting pulse and quicker return to resting level after exercise.
Stature: The short and thin persons have a more rapid pulse than tall and heavy.
Emotions: Anger or excitement increases the pulse rate temporally. When the stress gets heavy; we notice that our body naturally responds with a quickening pulse. The same goes for fear, another type of anxiety, which prompts the flight response and releases hormones that make the heart pump faster.
Fever: When body temperature is elevated, the pulse rate usually increases as well. A sudden change in temperature quicken heart rate as blood immediately rushes to skin's surface in order to cool or warm you up. Pulse increases at a rate of about 10 beats per minute each degree rise of body temperature (10:10).
Blood Pressure: When the blood pressure decreases, pulse rate may increase to increase the flow of blood. If blood pressure increases, pulse rate may decrease to correct the blood flow.
Drugs: Stimulant drugs increase the pulse rate. Depressant drugs decrease the pulse rate.
Disease Condition: When the body's immune system becomes compromised for example, with fever, injury, anemia, or infection changes in heart rate can occur. Particularly if septic shock, the heart rate will naturally quicken to meet oxygen demands. Heart disease, thyroid disease and other infections effect on pulse rate. Heart disease occurs due to plaque building up in the arteries, which leads to arrhythmias followed by heart attack or heart failure. This arrhythmia (or irregular heart beat) will cause muscle damage, which will result in a decreasing or quickening pulse.
Acute Pain and Anxiety: Increase pulse.
Severe and Chronic Pain: Decrease pulse.
Glycogen Levels: If the glycogen stored in the body diminishes, we will suffer fatigue. However, to properly fuel muscles, heart rate will naturally increase to boost your energy levels.
Dehydration: As we become increasingly dehydrated during a long walk, hike, or run, your blood becomes thicker and waste products build up in bloodstream so heart will work harder to maintain constant cardiac output. A fluid loss of 3% of body weight increases pulse rate because of decrease in circulating blood volume.
Pressure: Vagal stimulation (or pressure on the body's special sensors) occur during labor, a bowel movement, or if we lift a heavy object. The increased pressure causes the blood pressure to change and the heart often slows in response.
Hemorrhage: Loss of blood increases pulse rate because of demand of oxygen.
Position: Slow while lying down, and rapid while standing.
Scientific Principle for Taking Pulse
- Take the patient's pulse when they are at rest because exercise, feelings, and worry will all raise heart rate.
- The pulsation may be felt on touch-sensitive fingertip tips.
- The thumb should not be used to count pulses since it pulses, which might be mistaken for the patient's pulse.
- Take a minute to count your pulse, especially if it is erratic.
- The pace, rhythm, volume, and tension of the pulse are all variables that depend on the person and provide information about the heart's actions, the patient's health, and the nature of the blood vessels.
- Select a good location to take your pulse.
- If a patient is taking any medicine that might affect heart rate, nurses should be aware of it.
- Record pulse immediately.
- Always note the apical pulse for patients are with cardiovascular disease, on cardiac medications and critically ill.
Purposes
- to create baseline information.
- to look for irregularities in volume, rhythm, and pace.
- to keep track of any changes in the patient's health state.
- to evaluate the heart's reaction to cardiac drugs, activity, blood volume, and gas exchange.
- to examine the peripheral blood flow.
- to calculate the heartbeats per minute.
Articles Required
- Watch with second hand.
- Pen.
- Vital sign chart.
Things to remember
© 2021 Saralmind. All Rights Reserved.

 Login with google
Login with google