Overview of Nursing Process
Subject: Fundamentals of Nursing

Overview
Introduction
The nursing process is a scientific approach used by nurses to ensure patient care quality. It is a problem-solving method used by nurses to address patients' requirements. It is also a key blueprint for patient care. It is cyclical in the sense that each component of the nursing process follows a logical sequence, but multiple components may be involved at the same time. It establishes a framework for nursing accountability. The nursing process is also a standard of practice that, when followed correctly, shields nurses from legal issues associated with nursing care. It must be planned, client-centered, problem-oriented, goal-directed, dynamic, and ongoing.
Definition of Nursing Process
The nursing process is an organized and systematic approach of providing personalised care within the boundaries of nursing practice.
The nursing process can be defined as a systematic method of assessing the patient's need, planning care, implementing treatment, and evaluating the outcome of care provided. In nursing, it is a scientific and problem-solving approach.
The nursing process is a set of planned processes and actions aimed at addressing people's needs and solving their problems.
The nursing process is a critical thinking method used by professional nurses to apply the best available evidence to caregiving and improving human functions and responses to illness and health. - American Nurses Association, 2010.
Purposes of Nursing Process
- Determining a client's health status
- To assist nurses in identifying actual and potential health concerns, setting realistic goals, and intervening to individualize care.
- To provide optimal, need-based nursing care to clients in an efficient and informed manner.
- Encourage the identification and use of the client's strengths.
- To improve client and team member communication and interpersonal relationships.
- To improve care continuity by avoiding omissions and duplications of actions.
- To provide the client with scientifically based, holistic, personalised care.
Principles of Nursing Process
There are several fundamental principles that are vital to nursing practice and must be remembered when employing the nursing process.
- The patient possesses worth (value) and dignity (self-respect).
- There are a few fundamental prerequisites that must be accomplished. When these requirements are not met, problems arise that may involve the aid of another person until the individual is able to resume self-care.
- The patient is a unique individual who demands tailored care. Individual or unmet needs define the sort of nursing care required for every health issue.
- The patient and their family members are required to participate and are consulted on the care that will be provided.
- Nursing is a cyclical and continual activity.
- The patient has the right to quality nursing care that is offered with interest, compassion (sympathy), and competence, with an emphasis on wellness and prevention.
- During nursing care, the nursing team must communicate with one another.
- In this process, the therapeutic nurse-patient interaction is critical.
Advantages of Nursing Process in
For patients:
-
Individualized care: It is centered on the individual, treating each person as a unique being, and provides a framework for satisfying the requirements of the particular patient.
-
Holistic care: Because the care is personalized, the nurse can pay attention to the individual in all aspects of his health, resulting in a holistic plan of care.
-
Participation in the care: The utilization of the nursing process encourages the patient's active participation in his or her own health care. This type of involvement strengthens the patient's sense of control over what is occurring to him or her, encourages problem solving, and promotes personal responsibility. It increases the patient's commitment to achieving the specified goals.
-
Continuity of care: The use of the nursing process provides a common language for practice that clearly communicates the plan of care to coworkers and patients, thereby improving continuity of care and promoting the achievement of planned goals.
-
Quality of care/standards of care:It offers a structured, methodical technique of problem solving that reduces the risk of dangerous errors or omissions in caregiving. As a result, the quality of care improves.
For nurses:
-
Job satisfaction and professional growth: The nursing process distinguishes nursing as a distinct profession from that of physicians and other health professions. The utilization of the nursing process gives the nurse more control over their own practice. This increases the likelihood (possibility) of a favorable outcome by allowing them to apply their knowledge and expertise constructively (fruitfully). This, in turn, leads to increased job satisfaction and professional development.
- Confidence build up: It provides an organized, systematic method of problem solving and vehicle for evaluation which provides continuous feedback and helps to build up confidence.
-
Legal protection: As it provides an organized, systematic method of problem solving, it minimizes dangerous errors or omissions in care giving. It also acts as a good record and helps in legal protection.
-
Save energy and time: It acts as a means of communication and omits repetition in care thus saves time and energy.
-
Professional development: Enhances nursing efficiency by standardizing nursing practice.
Characteristics of Nursing Process
- Dynamic/Cyclical
- Systematic
- Client-centered
- Planned and data from each phase provide input into the next phase
- Use of critical thinking Focus on problem solving and decision making
- Critical thinking
- Interpersonal and collaborative
- Universally applicable
- Focus on problems or strengths
- Open, flexible
- Humanistic and individualized
- Outcome focused (results oriented)
- Emphasizes feedback and validation
Essential Abilities to Practice Nursing Process
Each of these steps requires different activities involving various abilities such as:
Cognitive Skills
Memory, the ability to learn new information, speaking, and comprehension of written material are all examples of cognitive skills. Cognition is concerned with how a person perceives and acts in the world. It is a set of abilities, skills, or procedures that are present in almost all human actions. Cognitive talents are brain-based capabilities that humans require to do any task, from the most basic to the most complicated. They have less to do with actual knowledge and more to do with the mechanisms of how we learn, remember, problem-solve, and pay attention. For instance, answering the telephone involves at least: perception (hearing the ring tone), decision taking (answering or not), motor skill (lifting the receiver), language skills (talking and understanding language), and social skills (interpreting tone of voice and interact- ing properly with another human being). So, nursing personnel must have the cognitive skill and other intellectual skills such as:
- Keen observation
- Critical thinking
- Making judgments
- Making decisions
- Applying knowledge from theory to practice
These abilities enable the nurses to offer a scientific rational for each element in the client's plan of care and also helps to select those nursing actions which most likely give desired outcomes.
Technical Skills /Abilities
The technical skill is that type of skill which is usually used in or peculiar to a specific field or profession which includes the following:
- Techniques and procedures
- Manual abilities
- Adaptation and improvisation
It enables nurses to manipulate equipment skillfully in order to achieve the desired result. Furthermore, it entails carrying out procedures in an appropriate or systematic manner.
Interpersonal Skills/ Abilities
Interpersonal skills are those skills which people use to properly interact with each other. Some of these basic skills include the following:
- Communication
- Interviewing
- Listening
- Teaching
- Team work
- Following direction, and Attitude
It enables nurses to establish and maintain caring relationships that aid in the achievement of desired goals by collaborating with the other health care team members as a respected and credible colleague to secure valued goals.
Components/Steps of Nursing Process
The nursing process is a scientific approach used by nurses to ensure patient care quality. Many authors have described the nursing process as having five basic steps: assessment, diagnosis, planning, implementation, and evaluation. These phases are abbreviated as "ADPIE." Practicing the five steps of the nursing process allows you to be organized and systematic in your practice.
Assessment
The first phase in the nursing process is assessment. It is the systematic and ongoing gathering, organizing, validating, and documenting of data. The planned and systematic collecting of data to evaluate a client's current and past health status, as well as the client's current and prior coping strategies, is known as assessment. During this phase, the nurse collects information about a patient's psychological, physiological, social, and spiritual status or conducts a comprehensive examination of the patient to determine his strengths and weaknesses, as well as his requirements and difficulties. It entails collecting both subjective and objective data.It is based on a broad scientific knowledge, keen observation and purposeful listening. It starts with the admission of patient and continuous while the patient is under the care of the nurse. Continuous assessment helps to modify the nursing care plan according to the changing needs of the patient. There are 4 different types of assessment.
Initial assessment: Performed within specified time after admission to a health care agency e.g. Nursing Admission Assessment.
Problem focused assessment: Ongoing process integrated with nursing care to determine specific problem identified in an earlier assessment and to identify new or overlooked problems e.g. assessment of a client's ability to perform self-care while assisting the client to bathe.
Emergency assessment: Done during psychiatric or physiological crisis of the client to identify life threatening problems e.g. rapid assessment of airway, breathing and circulation during cardiac arrest.
Time lapsed reassessment: Done several months after initial assessment to compare the client's status to baseline data previously obtained.
Purposes of Assessment
- To establish baseline information of the client.
- To determine the client's risk for dysfunction.
- To determine the client's strength.
- To provide data for the diagnosis.
- To identify the patient's problems.
Components of Assessment
Assessment consists of four separate activities:
- Data collection
- Data organization
- Data validation
- Documenting data
Data Collection
Data refers to the information gathered during the assessment process. Data are facts or realities expressed by the patient or collected in a methodical manner by health staff such as the nurse. The practice of acquiring information on a client's health status is known as data collection. The information gathered should be complete and concise. It should cover all aspects of the patient's care, such as physical, mental, social, and spiritual aspects, but flexibility is essential in data collection. Data can be gathered in a number of ways. In general, information is obtained from:
- Patient interview, physical tests, and general observation
- Reports and responses to interviews from family members or significant others
- Another member of the medical team
- Patients' histories, laboratory reports, x-rays, and interdisciplinary consultations are examples of medical record information.
- Scholarly literature
Types of Data
Subjective, symptomatic, or covert data: Subjective data consist of vocal descriptions of a patient's health issues. It is made up of information given to the nurse by the patient or his relatives, similar to taking a history. It is provided from the perspective of the patient or relative and is gathered during daily interactions with the individuals.
Objective data or signs or overt data: The information about the person obtained by the nurses through observation or physical examination and various tests which can be seen, heard, felt or smelled e.g. inspecting the condition of a surgical incision or wound, describing an observed behavior, discoloration of the skin and blood pressure readings are objective data. observer.on These data are considered objective because the data are found to be the same by any observer.
Sometimes, the data may be both subjective and objective. For example, swelling is subjective data because the patient tells the nurse about it. The nurse may check it and find that the patient has swollen legs. So it becomes objective data too. Whenever possible, subjective data should be validated with objective data too. After collecting subjective and objective data, the nurse may consult the seniors or the patient's chart to get the previous data [admission data] for comparison and for checking the consistency of the data. For a complete subjective data base, a total health history is necessary but sometimes the patient may come to hospital in an actually ill state. In such cases, the nurse should take only the specific health history related to the patient's complaint at the time of admission; detailed health history can be taken later. This is also the case for objective data. If the patient is brought into the emergency room with a bleeding wound, the nurse should not make the patient wait and do a total body assessment. In such cases, she should do an assessment of the specific area of complaint and later on, she should do the total body assessment as soon as possible because this is also may add useful information for the care of the patient.
Sources of Data
Primary sources: A client is the primary and best source of information. Verbal and nonverbal information from a patient is primary data. The patients who are conscious, alert, and be to answer questions correctly provide the most accurate information about their health care needs, lifestyle patterns, present and past illnesses, perception of symptoms, responses to treatment and changes in activities of daily living. The family members and significant others are considered as the primary source of information for infants or children, critically ill adults, mentally handicapped patients, or patients who are unconscious or have reduced cognitive function.
Secondary sources: In fact, all sources except the client are considered secondary sources. They can verify the findings of a patient e.g. does the patient take medications regularly at home? Has the patient's appetite changed over time, or how well does the patient sleep, etc.
Sources of secondary data are:
- Family members
- Client's records / documentation: it includes information documented by various health pe care professionals.
- Medical records e.g. medical history, physical examination, operation notes, progress notes, consultation done by physicians
- Records of therapies done by other health professionals e.g. social workers, dieticians, physical therapists
- Laboratory records
- Verbal report of other health care professionals
- Literature
Factor Affecting Data Collection
- Physical, mental and emotional state of the patient
- Culture and social background
- Functional ability of senses
- Past experiences associated with present situation
- Way of presentation of data by the client
- Way of perceiving the data by nurses
Methods of Data Collection/Assessment
- Interviewing/ history taking
- Physical assessment
- Observation
- Review of clinical record
- Consultation
History Taking
History taking is a type of interview that is used to collect relevant data from the patient. An interview is a conversation between two or more persons with some purposes. It is a part of the communication process. It is used to collect subjective data for the assessment. About 80% of the information in the assessment is obtained by history taking. The history of a patient is information gained by a physician/nurse by asking specific questions, either of the patient or of other people who know the person and can give suitable information with the aim of obtaining information useful in formulating a diagnosis and providing care to the patient.
The medically relevant complaints reported by the patient or others familiar with the patient are referred to as symptoms, in contrast with clinical signs, which are ascertained by direct examination on the part of medical personnel. Most health encounters will result in some form of history being taken. Medical histories vary in their depth and focus. For example, an ambulance paramedic would typically limit his history to important details, such as name, history of presenting complaint, allergies, etc. In contrast, a psychiatric history is frequently lengthy and in depth, as many details about the patient's life are relevant to formulating a management plan for a psychiatric illness.
Purposes
- To find out the patient's condition [present and past]
-
To eliminate confusion about the patient's identity and obtain the information required for contacting the patient if the need arises.
-
To provide you with an introduction to the patient and some indication his habits, life style and beliefs which may be explore in greater depth in the personal and social history.
-
To initiate a relationship based on recognition of the importance of informant's role in sharing in the care of the patient.
-
To support for nursing care.
- To support for diagnosis, treatment and management.
Required Equipment
- Patient's charts
- Pen/pencil
Guidelines
- Be dressed neatly and in a culturally acceptable way for the interview.
- Establish rapport with the patient; greet the patient warmly; create a friendly and congenial atmosphere; make him/her feel secure and free to talk.
- Maintain privacy. Room should be quiet, calm and separate.
- Arrange the seating in such a way that both the patient and nurse are seated at the same level facing each other.
- Show respect to the patient and his ideas. Call him by his name.
- Explain the purpose of the interview to the patient. Indicate the approximate amount of time required for the interview.
- Make conversation at the level of the patient's understanding.
- Be an attentive listener.
- Maintain eye contact to make the patient feel that you are listening to him/her
- Do not interrupt him/her in between unless she/he is moving off the point.
- Observe the patient's non-verbal clues such as feelings of anger, guilt, frustration, anxiety, etc. when she/he is talking.
- Use the history-taking format to collect information. Make notes in short sentences and make them brief as possible.
- Keep the data obtained in the interview confidential and share it with the appropriate health team members only.
- Always consider the setting for assessment and patient's condition. A patient experiencing acute symptoms in an emergency department will not offer as information as one who comes to an outpatient clinic for a routine checkup.
- An older adult requires more time than younger, and often multiple visits are required to gather a complete database.
- Let the patient, know what information will be shared and with whom it will be shared.
Basic Components for a Health History
1. Biological information or patient's identification data: Biographical information is factual demographic data about the patient. The patients name, age, sex, education, occupation, marital status, if married number of children, address, religion, types of insurance if available, guardian's name, ward, bed number, date of admission, in patient number, provisional diagnosis, date of discharge and date of interview, etc are included.
2. Chief complaint or reason for hospitalization/seeking health care: It is the main reason for coming to hospital or to seek for visiting a physician or hospital or for help usually a single symptom, occasionally more than one complaints e.g. chest pain, palpitation, shortness of breath, ankle swelling, etc. The patients describe the problem in their own words and it should be recorded in the patient's own words in a chronological order. For this, ask the questions such as what brings you here? For how long you are ill? When were you completely normal? Is this complaining for the first time or you have other episodes? How can I help you? What seems to be the problem? And write in this way: "I feel tired", "My throat hurts", "I have chest pain", "I feel nauseous", "I can't sleep", "I have a headache", since last 2 days, etc. Chief complaints typically follow the format of complains of/presenting with [complaint] x [duration for which this has been bothering the client]. It should be short/specific in one clear sentence and here are some examples.
C/o fever × 3days
C/o diarrhea × 2day
C/o abdominal pain × 1 day
3. Health history: The information in a patient's health history provides data on the b patients' health care experiences and current health habits.
a. Present health history
It is the elaborative form of the chief complains which should be chronological account of Sn the major problems for which the patient is seeking medical care. The present history should include the onset of the problem, the setting in which it developed, its manifestations and any treatments. The principal system should be described in terms of their location, quality, The quantity and severity and timing (i.e. onset, duration and frequency).
When assessing a patient with a symptom or health concern, the nurse uses symptom analysis to help the patient describe the problem fully. A method for obtaining a systematic and thorough assessment, the symptom analysis is easy to remember with the mnemonic device (is any learning technique that aids information retention. Mnemonics aims to translate information into a form that the brain can retain better than its original Wiform), OPQRSTA. The following questions serve as a guide for effective symptom analysis. Ask OPQRSTA for each symptom.
O = Onset of disease or symptoms: It means the time of starting of the symptom in the body.
P Proactive or palliative/Position/site: It means what are the causes of the symptoms?
What makes it better or worse?
First occurrence: What were you doing when you first experienced or noticed the symptom?
Recurrence: What seems to trigger the problem?
Q = Quality or quantity: It means how the symptom feels, looks or sounds. How much of it are you experiencing now?
Quality: How would you describe the symptom and how it feels, looks or sounds? Quantity: How much are you experiencing now so that it prevents you from performing activities? Is it more or less than you experience at any other time?
R = Regions, radiation, reliving or aggravating factors: It means where the symptom is
located. Does it spread?
Region: Where does the symptom occur?
Radiation: In the case of pain, does it travel another part of your body?
Reliving or aggravating factors- any activities or position.
R: Relationship to anything or other bodily function/position.
S = Severity: It means how the symptom rate is on a severity scale of mo with 10 being ush Stom vilanoias 90 motquiva signi the most extreme.
Severity: How bad is the symptom at its worst? Does it force you to lie down, or slow down? How it affects daily work/physical activities. Wakes him up at night, cannot sleep/do any work.
Course: Does the symptom seem to be getting better, getting worse or staying about the in same?
T = Timing: It means mode (form) of onset. (Abrupt or gradual), progression (continuous or intermittent - if intermittent ask frequency/nature). How often does it occur? Treatment received or/and outcome
A = Are there any associated symptoms?
List in a clear chronological order the details of the problems or problems for which the patient is seeking care. We will determine by interrogating the time line of:
- When did the patient's problem(s) begin?
- Where did the problem begin?
- What kinds of symptoms did the patient experience?
- Has the patient taken any treatment for the problem?
- Has the treatment had any effect on the patient or has the treatment not improved or altered the patient's condition?
- It is also important to determine if the problem(s) have affected the patient's lifestyle. That is, have the symptoms experienced because of the problem(s) caused any incapacity?
- Are there any associated symptoms?
b. Past health history
A comprehensive survey of a patient's past history which provides the information about patient's major health problems. Similarly, it also gives you an insight about the health status of the patient up until now. Ask the patient about the following elements of his/her previous major health problems or past history.
Past medical history
Ask the patient the following:
- About past hospitalization and reason of hospitalization, etc.
- Childhood illness: Measles, malnutrition, mumps, whooping cough, chicken pox, rheumatic fever, tuberculosis, polio, etc.
- Immunization: Complete, incomplete.
- Adult illness/previous illness such as IHD (ischemic heart disease), DM, asthma, TB, Jaundice, Fits and ask also in detail about each problem for example, if diabetic presented mention time of diagnosis/current medication/ clinic checkup, etc., medication taken at home including home remedies medicine taken by self or prescribed by doctor, etc.
- Medication history
- Allergies disorders: Any allergic reaction to food, drugs and others etc. if the patient has an allergy, note the specific reaction and treatment.
- Ask the date for health screening e.g. PAP smear, mammogram, prostate specific antigen, blood sugar, lipid profile, etc.
Past surgical/ operation history
Ask the patient the following:
- Any type of the surgery in the past e.g. asks time/place/what type of operation, etc.
- Injuries, trauma, accidents e.g. ask time/place/what type of injuries and trauma etc.
- Blood transfusion, etc.
4. Family history: The family history obtains data about immediate and blood relatives. It includes health history of the parents, grandparents, first uncles, aunts; brothers and sister include their state of health. After the patient's medical history has been explored, it is important to find out about the health of the immediate members of the family:
- One has to determine if certain common diseases run in the family i.e. does a familial arop pattern exist?
- In this part of the history, you have to determine the and health of the patient's age parents, grandparents, siblings, spouse and children, etc.
- If any member is deceased, the age and cause of death is established. The objectives are to determine whether the patient is at risk for illness of a genetic or familial nature and to identify areas of health promotion and illness prevention. The family history also provides information about family structure, interaction, support, and function that often is useful in planning care. Use written statement and a diagram record family history which is given below:
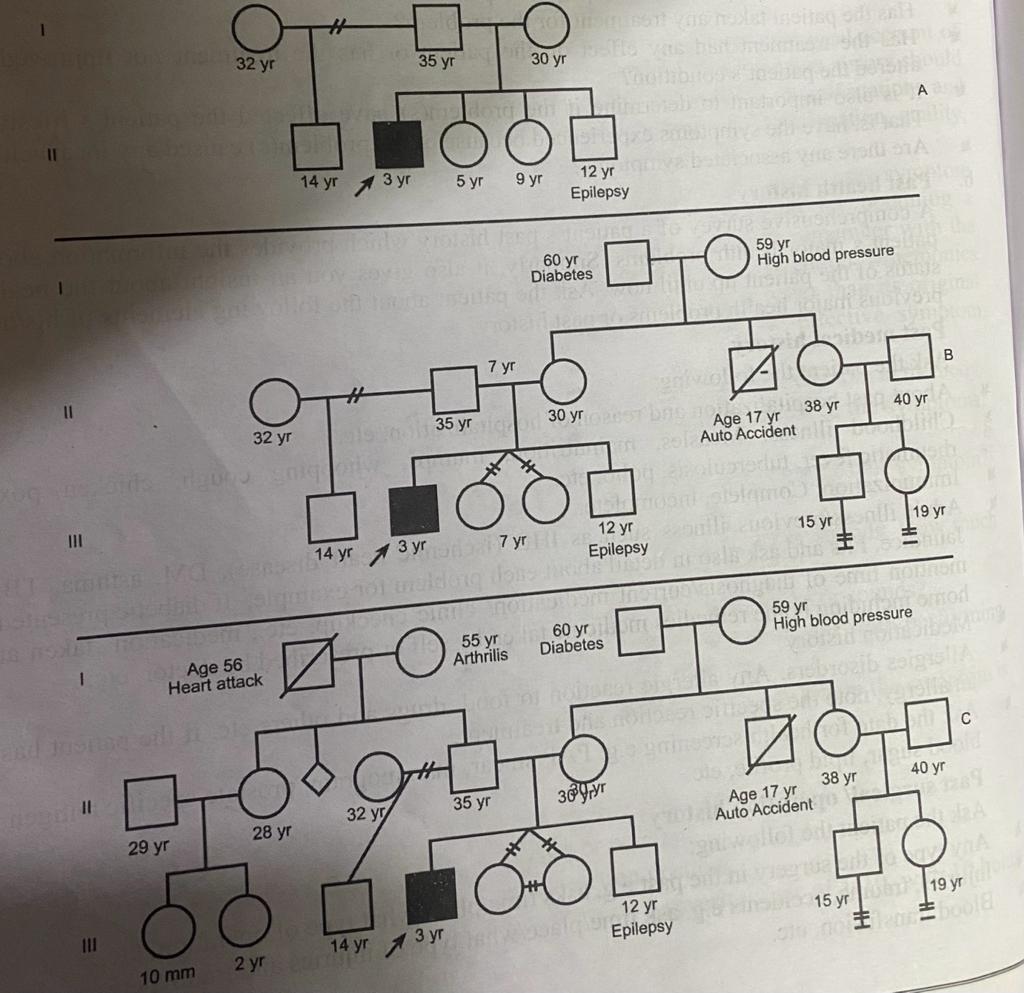
_1668598114.jpeg)
5. Personal history: In this part of the history, one tries to get an insight into the patient's lifestyle, occupation, and habits. In the lifestyle component, le component, an attempt is made to understand what constitutes a typical day for the patient.
- What does the patient do for recreation, relaxation, etc.?
- What kind of job does the patient have? Are there any job-related toxic exposures that exist?
- Is there any history of alcohol intake? How much? Coffee/tea intake? How much? Any history of diarrhea, vomiting?
- Is there any history of smoking cigarettes or using "recreational" drugs like marijuana, cocaine, amphetamines, etc.?
- Has the patient ever used IV drugs? Has he ever swapped needles?
- Has the patient been exposed to any infectious diseases or sexually transmitted diseases (STIs)?
6. Menstrual and obstetrical history: Date of LMP, regularity, duration, if married any Os contraceptive measures taken, number of living children, abortion, still birth, infertility, any history of menorrhagia, etc.
7. Psychosocial history: Social history includes the history of ethnicity, language spoken, educational status, occupation [type of job], housing (owning or renting shelter), type of family, adequacy of income, family relations, etc. A psychosocial history reveals the patients support system, which often includes spouse, children, other family members and close friends. The history includes information about ways that the patient and family typically cope with stress.
Environmental history: The environmental history provides data about a patients home and working environments with a focus on determining the patients safety. Information about the home environment includes function of utilities, layout of rooms in the house, and the presence of any barriers or risks for injury. Other information includes the source of drinking water, sanitation status at home and surroundings such as type of drainage system, type of toilet used, kitchen style, type of fuel used in cooking, etc. the history also identifies exposure to pollutants in the workplace, existence of high crime in the patients neighborhood.
9. Spiritual history: Life experiences and events shape a person's spirituality. The spiritual dimension represents the totality of ones being and is difficult to assess quickly. Review with patients their beliefs about life, their source for guidance in acting on beliefs, and the relationship they have with family in exercising their faith. Also assess rituals and religious practices that patients use to express their spirituality.
10. Review of systems (ROS): The review of systems is a systematic approach for collecting the patient's self-reported data on all body systems. In this portion of the history, all organ systems not already discussed during the interview are systematically reviewed. ROS is a final methodical inquiry, prior to physical examination. It provides a thorough search for further, as yet unestablished, disease processes in the patient. If the patient has failed to mention symptoms, this process of ROS would remind the patient at this point. Also, if you have unknowingly omitted certain points of inquiry, now would be the time to establish those. The following are the topics to be reviewed for each organ system:
Constitutional
- Any history of recent weight change
- Any history of anorexia (loss of appetite), weakness, fatigue, fever, chills, insomnia, irritability or night sweats
Skin
- Any history of allergic skin rashes
- Any itching of the skin
- Any history of unhealed lesions (probably due to: diabetes; poor diet; ster nd other causes of decreased immunity, especially AIDS)
- Any history of bruising, bleeding
Head
- Any history of headaches
- Loss of consciousness (may be due to cardiovascular, neurologic causes, anxiety, metabolic causes, etc.)
- History of seizures. Are they general (with or without loss of consciousness) or focal? Are there any motor movements?
- Is there any history of head injury?
Eyes
- Check for vision, history of glaucoma ( could cause pain in the eyes), redness, irritation, halos (seeing a white ring around a light source), blurred vision
- Any irritation of the eyes, excessive tearing, which can be associated with frequent allergic symptoms
Nose: Bleeding/blocking
Ears
- Any recent change in hearing?
- Any pain in the ears or ringing in the ears (tinnitus) or discharge?
- Any history of vertigo (dizziness)?
Lymph Glands
- Any history of lymph glandular enlargement in the neck or elsewhere? Are they tender/ painless? How they were first noticed?
- Are they freely mobile or are they adherent to the underlying tissues?
Respiratory System
- History of frequent sinus infections
- Postnasal drop Nosebleeds
- Cough (with/without expectoration)
- Color of sputum, when present
- History of sore throat
- History of shortness of breath on exertion or at rest
- Any history of wheezing (may be due to asthma, allergies, etc.)
- Hemoptysis (blood in the sputum): may be due to dental causes; lung causes like bronchitis, tuberculosis; cardiac causes like mitral stenosis or CHF (congestive heart failure). Determine if it is blood-tinged sputum or there is frank blood in the sputum.
- Any history of bronchitis, asthma, pneumonia, emphysema, etc.
Cardiovascular System
- History of chest pain or discomfort
- History of palpitations: were the palpitations associated with syncope (loss of consciousness)?
- History of either hypertension or hypotension
- Does the patient experience any paroxysmal nocturnal dyspnea (shortness of breath during sleep, in the middle of the night)? Is there any SOB (shortness of breath) in relation to exercise or exertion?
- Any history of orthopnea (shortness of breath when lying flat in bed)? Does the patient use more than one pillow to sleep? Has this always been the case, or has the patient recently started using more pillows?
- History of edema (site of edema- legs, face, etc.)
- Any history of leg pains, cramps? Are they relieved by rest (this is suggestive of intermittent claudication) or is it unremitting? (this is muscular)
- Any history of murmur(s), rheumatic fever, varicose veins?
- Any history of hypercholesterolemia, gout, excessive smoking i.e., conditions which can lead to or worsen heart disease
Gastrointestinal System
- History of bleeding gums, oral ulcers or sores
- History of dysphagia (can the patient point out and describe where the difficulty swallowing exists?)
- History of heartburn, indigestion, bloating, belching, flatulence
- History of nausea: Is it related to food? Is it one of the many symptoms due to GI (gastrointestinal) disease?
- Vomiting: Is there any associated weight loss, psychosocial factors, or are medications causing it?
- Hematemesis (vomiting blood). Ask for associated ulcer history, food intolerance, abdominal pain or discomfort.
- Jaundice: Is there a viral cause, gallstones, associated family history?
- History of diarrhea/constipation Any change in color of stools
Genitourinary
- History of polyuria (excessive urination) due to diabetes, renal disease, unknown cause etc. Check if this has been a recent change.
- History of nocturia (getting up at night to go to the bathroom). Is this a recent change?
- History of dysuria (painful urination). If it is because of urinary tract infection (UTI), the patient will experience frequency and urgency in addition to dysuria. STD will also be associated with similar symptoms (was treatment for STD completed?)
- History of renal stones, pain in the loins, frequent UTI
Musculoskeletal System
- History of joint pain- determines location: Is it acute or chronic? Unilateral or bilateral?
- More in the morning or evening? Are there associated systemic symptoms?
- Any history of rheumatoid arthritis, osteoarthritis, gout, etc.
Endocrine System old
- History of symptoms due to diabetes, i.e., polyuria, polydipsia, polyphagia, weight change.
- History of thyroid symptoms: heat/cold intolerance, increased/decreased heart rate, goiter, etc.
- History of adrenal symptoms: weight change, easy bruising, hypertension, etc.
- Polyuria-excessive urination; polydipsia-excessive thirst; polyphagia-excessive appetite.
Nervous System
- History of stroke, CVA, etc.
- History of muscle weakness, involuntary movements: they may be tremors, seizures, or anxiety, etc.
- History of sensory loss of any kind: anesthesia, paresthesias, or hyperesthesias.
- Anesthesia - no sensation; paresthesia → altered sensation, commonly a pins and -> needles sensation; hyperesthesia → increased sensation.
- Is there any change in memory, especially recent change?
11. Summary of history/concluding history: Conclude the health history by summarizing all findings. If interview (history taking) points out a significant health problem tell the patient what it is. What to be expected and what can be done about it?
Documentation of history findings: As u conclude the nursing health history, record the assessment data in a clear, concise manner using appropriate terminology. Standardized forms make it easy to enter data as the patient responds to questions. Record should be clear and concise record.
Inhibiting Factors of History Taking
Factors that inhibit a proper medical history taking include physical inability of the patient to communicate with the physician/nurse, such as unconsciousness and communication disorders. In such cases, it may be necessary to perform a so-called heteroanamnesis of other people who know the person and can give suitable information, which, however, generally is more limited than a direct anamnesis (a patient's account of their medical history). Medical history taking may also be impaired by various factors impeding a proper doctor/nurse -patient relationship, such as transitions to physicians/nurses that are unfamiliar to the patient.
History taking of issues related to sexual or reproductive medicine may be inhibited by an unwillingness of the patient to disclose intimate or uncomfortable information. Even if such an issue is on the patient's mind, he or she often doesn't start talking about such an issue without the physician initiating the subject by a specific question about sexual or reproductive health. Some familiarity with the doctor/nurse generally makes it easier for patients to talk about intimate issues such as sexual subjects, but for some patients, a very high degree of familiarity may make the patient reluctant (unwilling) to reveal such intimate issues. When visiting a health provider about sexual issues, having both partners of a couple present is often necessary, and is typically a good thing, but may also prevent the disclosure of certain subjects, and, according to one report, increases the stress level.
Physical Examination
Physical examination is an important tool in assessing the patient's health status. About 15% of the information used in the assessment comes from the physical examination. Physical examination is systematic collection of objective information that is directly observed or is elicited through examination techniques. It is a systematic data collection method that uses the senses of sight, hearing, smell, and touch to detect health problems.
The information obtained must be thoughtfully integrated with the patient's history and pathophysiology. Moreover, it is a unique situation in which patient and physician/nurse understand that the interaction is intended to be diagnostic and therapeutic. The physical examination, thoughtfully performed, should yield 20% of the data necessary for patient diagnosis and management.
Purposes of Physical Assessment
- To obtain baseline data about the client's functional abilities.
- To obtain data that will help the nurse establish nursing diagnosis and plan the client's care.
- To evaluate the physiologic outcomes of health care and thus the progress of a client's health problem.
- To make clinical judgments on a client's health status.
- To determine the client's eligibility [suitable fitness] for health insurance, military service or a new job.
- General Guidelines/principles for Physical Examination
Always stress the word ("WIPER")
W-Wash your hands.
I - Introduce yourself to the patient
P - Permission. Explain that you wish to perform an abdominal examination and obtain consent for the examination.
Pain: Ask the patient if they are in any pain and to tell you if they experience any during the examination.
E- Expose the necessary parts of the patient. Ensure adequate privacy.
R-Reposition the patient. In this examination the patient should be lying flat with one pillow under the head. This is not possible with all patients so first check if they are comfortable in this position.
Note: As the environment affects the quality of the physical examination, it is wise to arrange for quiet and privacy, optimum lighting the room for parts of the examination, and comfort for the patient and examiner.
The complete examination should proceed in an orderly fashion with a minimum of required Generally cephalocaudal approach is used, but in case of infant and child, examination of heart and lungs function should be done before the examination of other body parts, because as the infant starts crying, his/her respiratory and heart rate may change.
position of the patient and examiner during the physical examination
| Anatomical area or activity | patient | examiner |
| vital signs, general inspection | sitting or reclining (lie down) | standing before patient or at right bed side |
| head and neck | sitting | standing before patient |
| anterior torso(trunk) | sitting | standing before patient initially later behind the patient |
| posterior torso | sitting | at patient's side |
| anterior chest and abdomen | supine | before the patient |
| male genitalia | standing | before the patient |
| gait, station, coordination | variable positions | before the patient |
| female genitalia | lithotomy or dorsal recommend | sitting on chair st times or standing |
Methods of Physical Examination
A systematic approach should be used while doing physical examination. This helps to avoid duplication or omission. Generally cephalocaudal approach e.g. head to toe approach is used. But flexibility may be used as per the need of the patient. The procedure can vary according to the age of the individual, the severity of the illness, the preferences of the nurse, location of the examination and the agency's priorities and procedures. The sequence of the assessment differs with children and adults.
In a small child, examination of heart and lungs' functions may be done before the examination of other body parts, because once the child starts crying, his breathing and heart rate may change. The commonly used methods of physical examination are change. The commonly used methods of physical examination are:
- Inspection
- Palpation
- Percussion
- Auscultation
- Clinical measurement
- Smelling
Inspection
Inspection is the visual examination, which is assessing by using the sense of sight to discover some signs of illness. The nurse inspects with the naked eyes and with a lighted instrument such as an otoscope [use to view the ear]. Visual inspection helps to assess moisture, colour and texture of the body surfaces as well as shape, position, size, colour and symmetry of the body. Inspection reveals more information than other method and is therefore the most useful method of physical examination.
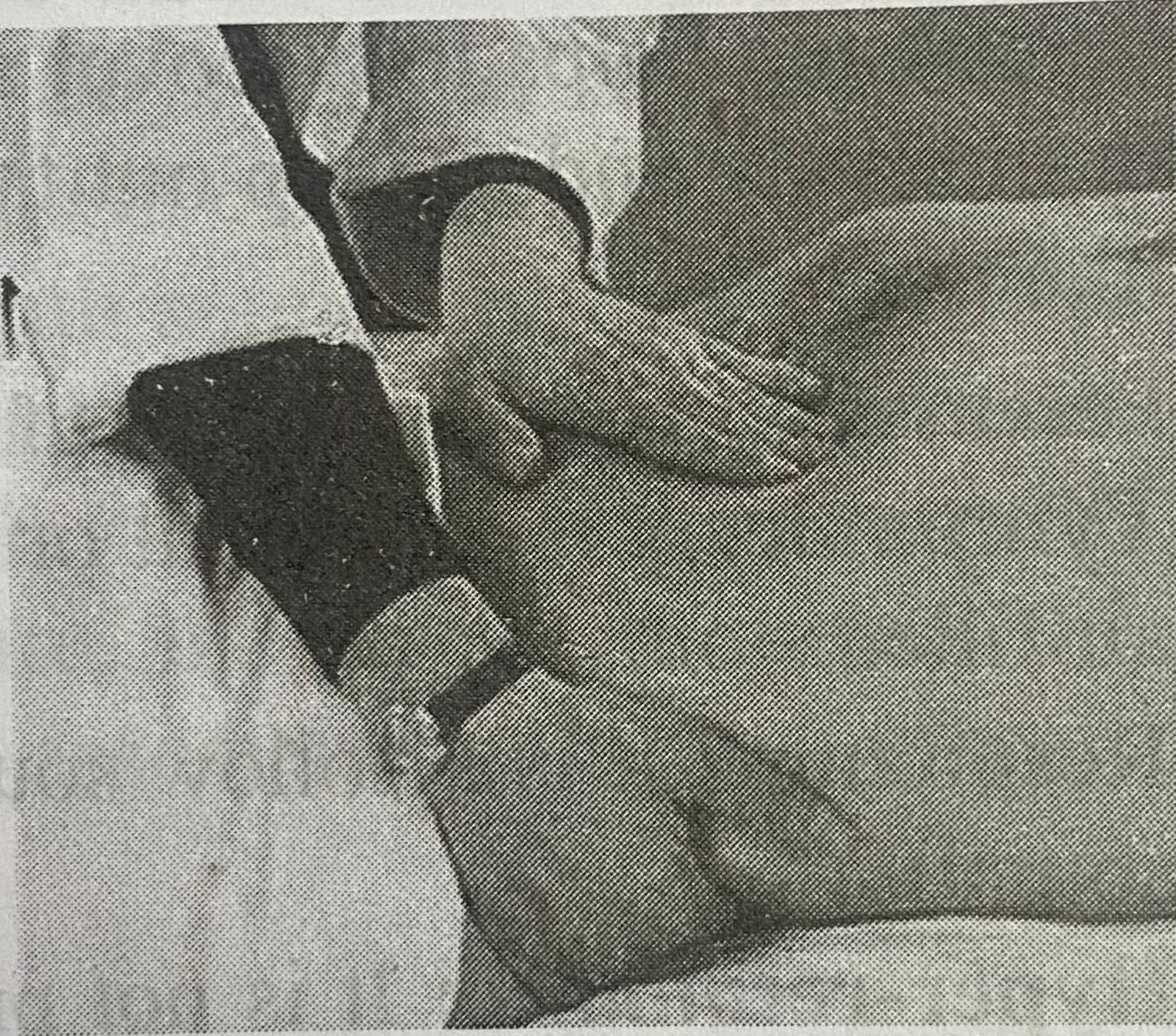
Palpation
Palpation follows inspection. It is the examination of the body using the sense of touch. Different parts of the hands are used for different sensations such as temperature, texture of skin, vibration, tenderness, etc. Finger tips are used for fine tactile details, the back of fingers for temperature and the flat of the palm and fingers for vibrations such as cardiac thrill. All the accessible parts of the body should be palpated. Palpation may be either light or deep and is controlled by the amount of pressure applied to the fingers or hand.
Light palpation is done with the hand parallel to the floor with the fingers together as in palpating the abdomen. The palm lies lightly on the part and the fingers depress the part about ½ or 1 cm deep. Light palpation of structure such as the abdomen determines the areas of tenderness. Deep palpation is performed by pressing the distal half of the palmer surface of the fingers into the abdominal wall. It is used to examine the condition of organs. It also helps to obtain more specific information about the mass detected by light palpation
- Palpation is used to determine:
- Texture e.g. the hair
- Position e.g. size, consistency, and mobility of organs or masses
- Distention e.g. of the urinary bladder
- Vibration e.g. of a joint
- Pulsation and
- the presence of pain upon someone
Principles of Palpation
- You should have short fingernails.
- You should warm your hands prior to placing them on the patient.
- Encourage the patient to continue to breathe normally throughout the palpation.
- If pain is experienced during the palpation discontinue the palpation immediately.
- Inform the patient where, when, and how the touch will occur, especially when the patient cannot see what you are doing.
Percussion
Percussion is the act of striking the body surface to elicit sounds that can be heard or vibrations that can be felt when they are tapped with the fingers. There are two types of percussion.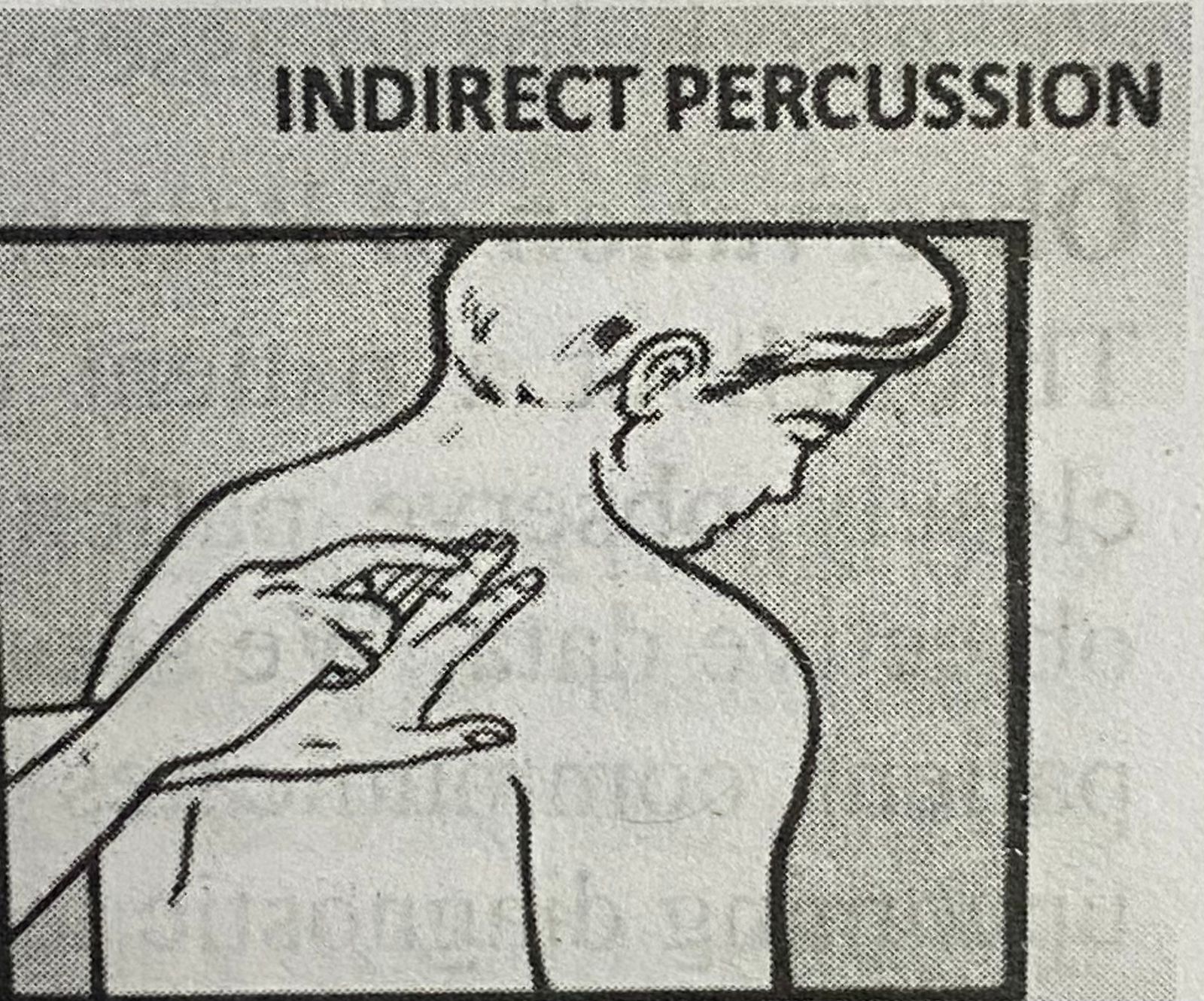
Direct percussion: It strikes the area to be percussed, directly with the pads of two, three or four fingers or with the pad of the middle finger.Indirect percussion: It is the striking of an object e.g. A finger held against the body area to be examined. In this technique, the middle finger of the non-dominant hand, referred to as the pleximeter, is placed firmly on the client's skin.
In order to do percussion the nurse should:
- Put the middle finger of her left hand against the body part to be percussed.
-
Tap the end joint of this finger with the middle finger of the right hand. Move the right hand from the wrist to tap the left middle finger.
-
Give two or three taps at each area to be percussed.
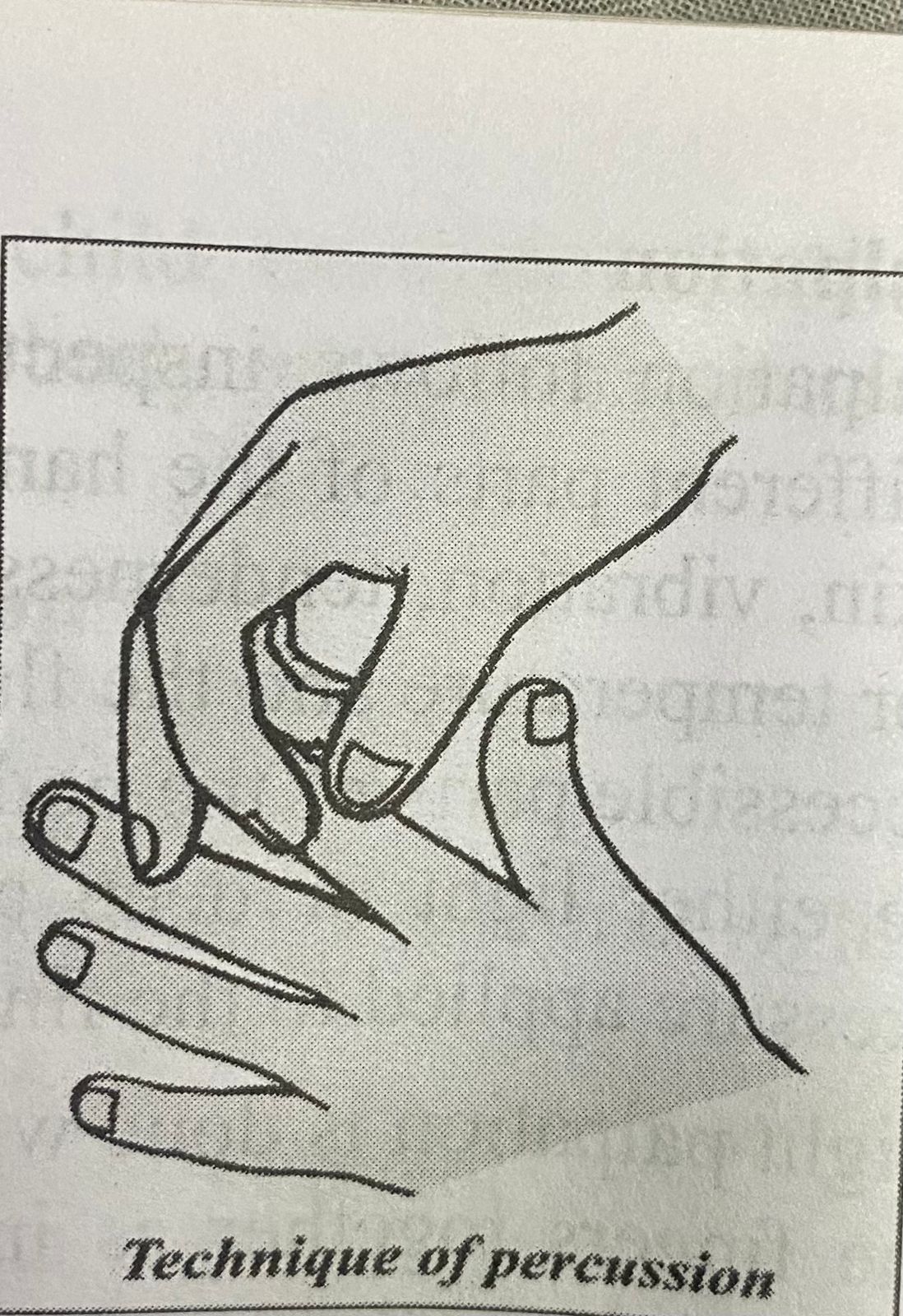
-
Compare the sound produced at different areas.
Percussion helps to discover abnormal solid masses, fluid and gas in the body and to map out the size and borders of certain organs like the heart.
Percussion produces 5 types of sounds
Tympanic: It is a musical or drum- like sound produced from an Technique of percussion air filled stomach.
Resonance: It is a hollow sound such as that produced by lungs filled with air. (Normal lungs
sound)
Hyper-resonance: It is not produced in the normal body. It is described as booming and can be heard over the emphysematous lungs.
Dullness: It is the thud like sound produced by dense tissue such as the liver, spleen, heart, etc. Flatness: Flatness is an extremely dull sound produced by very dense tissue, such as muscle or bone.
Auscultation
Auscultation means listening to the sounds transmitted by a stethoscope. The stethoscope is used to listen to the heart, lungs and bowel sounds. Auscultation may be direct or indirect:
- Direct auscultation is the use of the unaided ear for example, to listen to a respiration wheeze or the grating of a moving joint.
- Indirect auscultation is the use of a stethoscope, which amplifies the sounds and conveys them to the nurse's ears.
the stethoscope should always be placed on naked skin because clothing obscures sounds. It requires concentration and practice. Closing your eyes may help to focus on a particular sound.
Smelling
Smelling means discovering the odours given off by various parts of the body. The nurse should smell the patient's breath and other body discharges like sputum, vomitus, faece, urine, etc. to detect unusual odours, which may indicate any abnormalities.
Clinical measurement
Clinical measurement such as height, weight, blood pressure, temperature, pulse, respiration, etc. also helps to assess the patient's physical status.
Observation of Patient Behavior
Throughout a patient centered interview and physical examination it is important for u to closely observe patient's verbal and nonverbal behaviours. The information adds depth to objective data. We should learn to determine if data obtained by observation matches what the patient communicates verbally. For example, if a patient expresses no concern about an upcoming diagnostic test but show poor eye contact, shakiness, and restlessness, all suggesting anxiety, verbal and nonverbal data conflict. Observation directs to gather additional objective information to form accurate conclusions about the patient's condition.
And important aspect of observation includes a patient's level of function such as the physical, developmental, psychological, and social aspects of everyday living. Observation of level of function involves watching what a patient does such as eating or making a decision about preparing a medication rather than what the patient tells you he she can do.
Diagnostic and Laboratory Data
The results of diagnostic and laboratory tests provide further explanation of alterations or nursing health history and physical examination. For ex example problems identified during during the history the patient reports having a bad cold for 6 days and at present has a productive cough with brown sputum and mild shortness of breath. On examination you notice an elevated temperature, increased respirations, and decreased breath sounds in the right lower lobe. You review the results of a complete blood count and note that the white blood cell count is elevated. After that you report physician who orders a chest x-ray film. When the results of the x ray ray film show the presence of a right lower lobe infiltrate, the physician makes the medical diagnosis of pneumonia. Nurse's assessment leads to the associated nursing diagnosis of impaired gas exchange.
Organization of Data
After collecting the data, the data must be organized to make it meaningful. Various methods may be used to organize data. Abraham Maslow, a psychologist has given a method for data organization. According to him, all human beings have some basic needs, which can be placed in a hierarchical order. Primary or physiological needs are placed at the bottom of the hierarchy and secondary or non-physiological needs are placed at the top level of the hierarchy.
Here is an example of organizing data using Maslow's hierarchy of needs.
Physiological needs sviss
- The patient has 390C temperature.
- No bowel movement for 2 days.
Safety and security needs
- Worried about surgery
- Afraid of being alone in the room
Love and belonging needs
- wife is rooming - in- with him
- I am missing children.
Self-esteem needs
- "I need to be fed like children".
- "I do not think I will be able to walk again like children".
After collecting data, they should be reviewed for any omissions, incompleteness inconsistency. If the data are missing go back to the patient and collect the additional data.
Validation of Data
Validation of assessment data is the comparison of data with another source to determine data accuracy. It is double checking or verifying the data is accurate and factual. The information gathered during assessment phase must be complete, factual and accurate because the nursing diagnoses and interventions are based on this information. Validate findings from the physical examination and observation of patient behavior by comparing data in the medical record and consulting with other nurses or health care team members. Validating data helps the nurse ensure that assessment information is complete and ensures that objective and related subjective data agree. Always should obtain additional information that may have been overlooked and avoid jumping to conclusions and focusing in the wrong direction to identify problems.
Documentation of Data
To complete the assessment phase, the nurse records the client's data. The timely, through and accurate documentation of facts required in recording patient data. Data are recorded in a factual manner and not interpreted by the nurse e.g. the nurse records the client's breakfast intake [objective data] as coffee 240 ml, 1 egg and 1 slice of toast rather than as “appetite good". The nurse records subjective data in the client's own words. Accurate documentation is essential to communicate the information of the patient and should include all data collected about the client's health status and record all nursing care interventions and their outcomes.
Things to remember
© 2021 Saralmind. All Rights Reserved.

 Login with google
Login with google