Cardiomyopathy
Subject: Medical and Surgical Nursing I (Theory)

Overview
Cardiomyopathy is a heart muscle illness or disease that can be transient or chronic and cause cardiac dysfunction (heart loses effectiveness as a pump).
The heart muscle enlarges, thickens, or becomes hard when there is cardiomyopathy. The heart weakens and is less able to pump blood through the body and maintain a regular electrical rhythm as the condition worsens. Arrhythmias or heart failure may result. Due to a weak heart, issues can also occur with the heart valves.
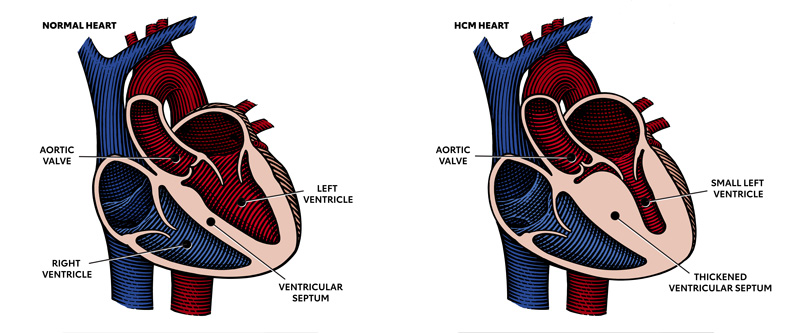
- Hypertrophic cardiomyopathy: Massive ventricular hypertrophy, C.O is normal, ↑ inflow resistance, and mitral valve incompetence, arrhythmais and sudden death
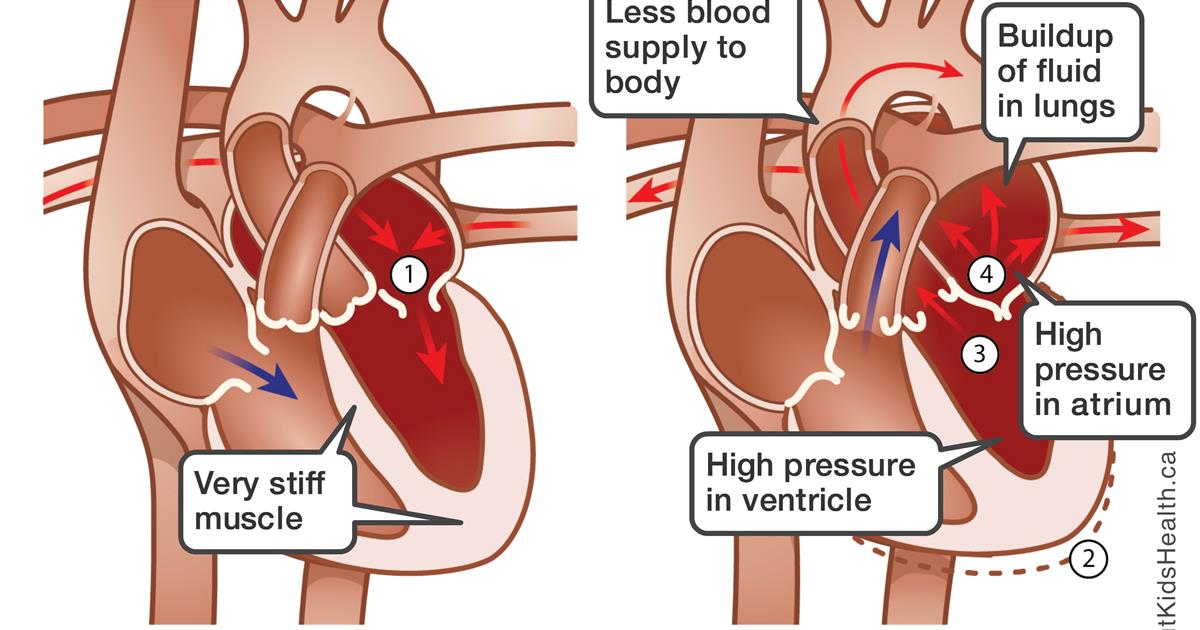
- Restrictive Cardiomyopathy: Restriction of filling of the ventricles or reduced diastolic compliance of the ventricle. C.O is normal or ↑ formation of thrombi, dilation of left atrium, and mitral valve incompetence.
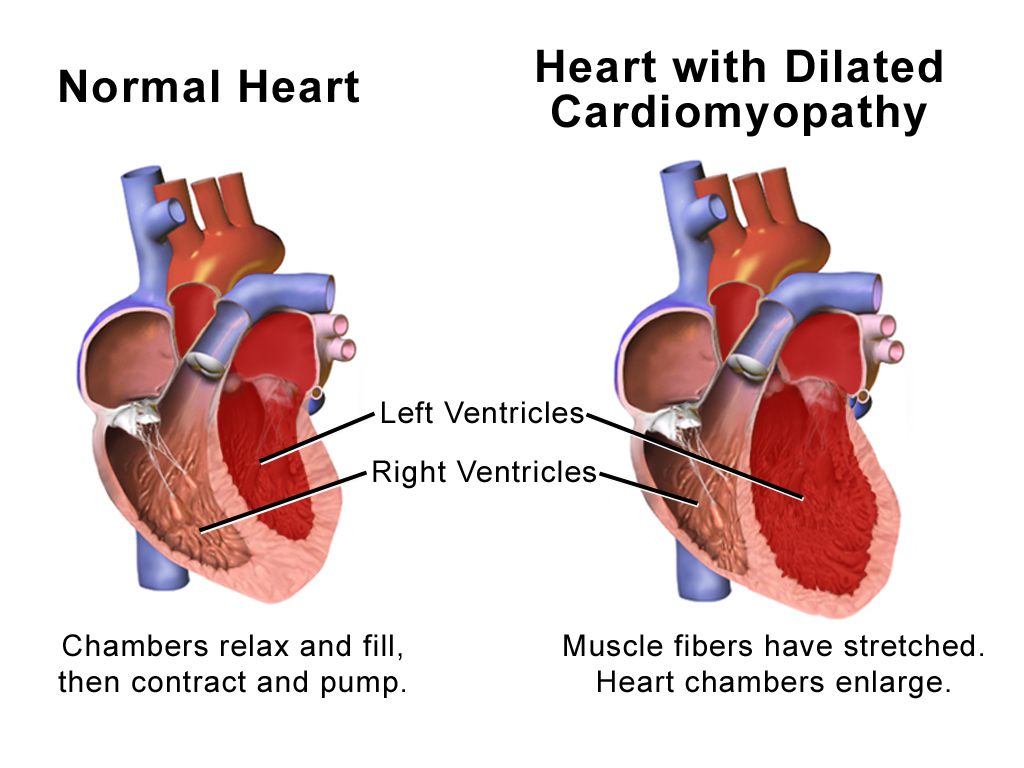
- Dilated Cardiomyopathy: The most prevalent form of cardiomyopathy, dilated cardiomyopathy (DCM), is characterized by ventricular enlargement, contractile dysfunction, and heart failure. A heart chamber enlarges or dilates as a result of diseased muscle fibers being stretched.
Pathophysiology
- All cardiomyopathies have a common pathogenesis, which is a chain of actions that leads to diminished cardiac output.
- The sympathetic nervous system and the renin-angiotensin-aldosterone response are stimulated by decreased stroke volume, which increases systemic vascular resistance, salt and fluid retention, and the heart's workload.
- Heart failure can result from these changes.
- Weakened, unusually enlarged, thickened, or rigid cardiac muscle are some of the symptoms. Heart failure results from the heart's inability to pump blood to the body's other organs.
- Loss of blood pumping capacity and, occasionally, disturbances in heart rhythm cause dysrhythmias, or irregular heartbeats.
- The illness usually gets worse over time, and occasionally it does so quickly.
Signs and Symptoms of DCM
- Left ventricular failure signs
- intolerance to activity
- Fatigue and weakness
- chest pain
- Dysrhythmias
- Eventually, right ventricular failure symptoms
Diagnosis
- Heart disease in the family and medical history A physical examination can reveal accumulation, which is a symptom of heart failure, as can swelling in the ankles, feet, abdomen, or neck veins.
- Holter monitoring, ECG, and a chest X-ray
- cardiac catheterization, coro angiography, and echocardiography
- Cardiovascular Biopsy
Treatment
alleviate heart failure symptoms, cut back on work and anticoagulants, and organ transplants. Treatment consists of Symptom management alleviates symptoms
- To improve cardiac output, diuretics, cardiac glycosides, and vasodilators are used.
- Dysrhythmias are treated using antidysrhythmics.
- Tell the patient to report any symptoms of dizziness or fainting, as these could be signs of a dysrhythmia.
- Tell the patient to avoid taking because it has a cardiac-depressant effect.
- Heart transplantation might be required.
Nursing Management of Cardiomyopathy
Assessment
- Throughout the phase, take your vital signs every 15 minutes.
- Every hour and as clinically indicated, monitor the patient for changes in their neurologic function. Check the capillary time, skin color, and warmth.
- In order to rule out myocardial ischemia, check for chest discomfort.
- To gauge the severity of heart failure, listen to your heart and lungs.
Monitor the Patient
- Obtain Bp at least once every hour because of the patient's unstable condition.
- To assess the effects of the pharmacologic intervention for the decreased cardiac output, check urine output every hour.
- Keep an eye on the patient's activity and avoid any interventions that could harm oxygenation.
- uPlse oximetry should be continuously monitored for oxygen levels.
- ECG rhythm strip analysis should be done at least four times a day.
Other Management
- To maintain or improve oxygenation, administer oxygen at a rate of 2 to 4 L/min,
- Remain well-rested to reduce your need for oxygen.
- Drugs should be given as directed.
- Offer a liquid diet throughout the acute phase,
- prior to and following the treatment of loop diuretics, check serum potassium levels.
- To avoid pressure sores, give your skin the care it needs.
- To reduce preload and afterload, take a diuretic as directed.
Things to remember
© 2021 Saralmind. All Rights Reserved.

 Login with google
Login with google